Affecting about 1 in 5,000 people worldwide, Marfan syndrome is far more than just being tall or having long fingers. As a cardiologist who has spent over a decade caring for patients with this condition, I have seen firsthand how it can range from a manageable health challenge to a serious, life changing disability. The truth is, Marfan syndrome is not automatically classified as a disability. However, when it substantially impairs major life activities, particularly through cardiovascular complications, it can certainly qualify as one.
In this comprehensive guide, We will walk you through everything you need to know about Marfan syndrome and disability. We will explore what this condition actually is, why the heart is so central to understanding its impact, and how disability is defined from both medical and legal perspectives.
Whether you are living with Marfan syndrome, caring for someone who is, or simply seeking reliable information, this article will provide you with evidence based insights to help you make informed decisions about your health and future.
What Is Marfan Syndrome?
Marfan syndrome is a genetic disorder that affects the connective tissue throughout your body. Think of connective tissue as the glue that holds your body together. It provides support and structure to your organs, blood vessels, bones, and other vital systems. When this tissue does not work properly, it can affect multiple parts of your body at once.
The Genetic Basis
The condition is caused by mutations in a gene called FBN1, which provides instructions for making a protein called fibrillin. This protein is a critical component of the microfibrils that form the structural framework of connective tissue. When fibrillin is abnormal, it leads to excessive signaling of a substance called transforming growth factor beta (TGF beta), which contributes to many of the features seen in Marfan syndrome.
About 75% of people with Marfan syndrome inherit it from a parent who has the condition. The inheritance pattern is called autosomal dominant, which means you only need one copy of the abnormal gene to develop the syndrome. If you have Marfan syndrome, there is a 50% chance of passing it to each of your children. The remaining 25% of cases occur due to new spontaneous mutations in people with no family history of the disorder.
It is important to note that Marfan syndrome does not affect intelligence. People with this condition have normal cognitive abilities and can excel in academic and professional pursuits.
Common Signs and Symptoms
Marfan syndrome affects multiple body systems, and symptoms can vary widely from person to person. Some individuals have mild features, while others experience more severe manifestations. Here is a breakdown of how different systems can be affected:
| System Affected | Common Symptoms |
| Skeletal | Tall, thin build; unusually long arms, legs, and fingers; scoliosis (curved spine); chest deformities (sunken or protruding breastbone); flat feet; flexible joints |
| Ocular (Eyes) | Lens dislocation (ectopia lentis); severe nearsightedness; increased risk of glaucoma and early cataracts; retinal detachment |
| Pulmonary (Lungs) | Spontaneous lung collapse (pneumothorax); sleep apnea; emphysematous changes in the lungs |
| Skin | Stretch marks (striae) without weight changes; tendency for recurrent hernias |
| Other | High arched palate; crowded teeth; dural ectasia (widening of the spinal canal covering) |
Cardiovascular Complications
As a cardiologist, I cannot emphasize this enough: the cardiovascular system is where Marfan syndrome poses its greatest dangers. Research shows that approximately 76% of adults with classic Marfan syndrome develop aortic dilation, while around 62% to 79% experience mitral valve prolapse. These cardiovascular complications are responsible for more than 90% of deaths related to this condition when left untreated.
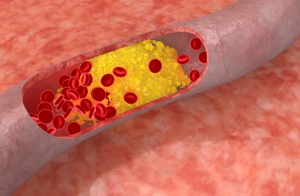
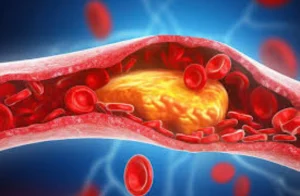
Aortic Problems: The Primary Concern
The aorta is the largest artery in your body, carrying oxygen rich blood from your heart to the rest of your body. In Marfan syndrome, the weakened connective tissue causes the aorta to gradually enlarge, particularly at its root where it connects to the heart. This progressive dilation creates several serious risks:
Aortic Aneurysm: The wall of the aorta bulges outward like a weak spot on a tire. This bulging weakens the vessel wall and increases the risk of rupture.
Aortic Dissection: This is a medical emergency where the inner layer of the aorta tears, allowing blood to flow between the layers of the vessel wall. Symptoms include sudden, severe tearing pain in the chest or back. Without immediate treatment, this condition can be fatal.
Aortic Regurgitation: As the aortic root enlarges, the aortic valve may no longer close properly, causing blood to leak backward into the heart. Over time, this places extra strain on the heart and can lead to heart failure.
Heart Valve Issues
Mitral Valve Prolapse (MVP): This occurs when the valve between the left upper and lower chambers of the heart does not close properly. The valve leaflets bulge (prolapse) into the upper chamber during heartbeat. While MVP alone is often harmless, in Marfan syndrome it can progress to significant mitral regurgitation, where blood leaks backward through the valve. Research indicates that mitral valve dysfunction is present in up to 79% of patients with Marfan syndrome. Symptoms may include palpitations, shortness of breath, fatigue, and chest discomfort.
Other Cardiovascular Concerns
Beyond the major issues, people with Marfan syndrome may also experience tricuspid valve problems, pulmonary artery dilation, and heart rhythm abnormalities (arrhythmias). Some studies have found an increased risk of ventricular arrhythmias, which in rare cases can contribute to sudden cardiac death. This is why regular cardiovascular monitoring is absolutely essential for anyone with this condition.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsDefining Disability in Legal and Medical Perspectives
Understanding whether Marfan syndrome qualifies as a disability requires looking at both medical and legal definitions. The answer is not straightforward because it depends on how severely the condition affects an individual’s daily life and ability to work.
The Medical Perspective
From a medical standpoint, disability occurs when symptoms significantly limit a person’s ability to perform daily activities. For someone with Marfan syndrome, this might mean experiencing such severe fatigue from heart problems that they cannot maintain regular employment, having vision loss that impairs their ability to read or drive, or dealing with chronic pain from skeletal abnormalities that limits mobility. The key factor is functional limitation: how much does the condition interfere with what you need to do in everyday life?
Americans with Disabilities Act (ADA)
The ADA does not maintain a specific list of conditions that automatically qualify as disabilities. Instead, it defines disability as a physical or mental impairment that substantially limits one or more major life activities. Major life activities include walking, breathing, seeing, working, and performing manual tasks. For someone with Marfan syndrome, cardiovascular limitations that affect breathing, exercise tolerance, or the ability to perform physical work could qualify under the ADA. The Job Accommodation Network notes that people with Marfan syndrome may develop various limitations, though the degree varies significantly among individuals.
Social Security Disability Benefits
The Social Security Administration (SSA) does not have a specific listing for Marfan syndrome in its Blue Book of qualifying conditions. However, this does not mean you cannot receive benefits. People with Marfan syndrome can qualify under listings associated with their specific complications, such as cardiovascular impairments (including aortic aneurysm under listing 4.10), vision loss, or musculoskeletal disorders.
To qualify, you must demonstrate that your condition prevents you from working at any job for at least 12 consecutive months. Medical evidence is crucial here. Documentation should include echocardiograms showing aortic enlargement or valve dysfunction, cardiac imaging studies, records of surgical interventions, and physician statements describing your functional limitations.
An important development is that Neonatal Marfan Syndrome, the most severe form affecting infants, is now included in the SSA’s Compassionate Allowances program. This allows for expedited approval of disability benefits for these critically affected individuals.
Management, Treatment, and Preventing Disability
One of the most encouraging aspects of Marfan syndrome care is how much we can do to prevent complications and preserve quality of life. With proper management, many people with this condition lead active, fulfilling lives without experiencing significant disability.
Diagnosis
Accurate diagnosis is the first step. The revised Ghent criteria, established in 2010, provide a standardized approach to diagnosing Marfan syndrome. Diagnosis typically involves clinical evaluation looking for characteristic features, echocardiography to assess the heart and aorta, eye examination by an ophthalmologist, genetic testing for FBN1 mutations (found in about 83% of genotyped individuals with confirmed Marfan syndrome), and family history assessment.
Medical Treatment
The cornerstone of medical treatment focuses on protecting the aorta and slowing its enlargement:
Beta Blockers: Medications like atenolol have been the standard treatment for decades. They work by reducing heart rate and blood pressure, thereby decreasing stress on the aortic wall. Research shows they help slow the rate of aortic dilation.
Angiotensin Receptor Blockers (ARBs): Medications like losartan and irbesartan have shown promising results. A landmark collaborative analysis published in The Lancet involving over 1,400 patients demonstrated that ARBs reduce the rate of aortic root enlargement by approximately half. This effect appears to be additive when combined with beta blockers, meaning combination therapy may provide even greater protection.
Important Note: Calcium channel blockers should generally be avoided in Marfan syndrome, as both animal and human studies suggest they may increase the risk of aortic complications.
Surgical Intervention
When the aorta reaches a critical size (typically around 5 cm, though this varies based on individual factors), preventive surgery is recommended. Elective aortic root replacement has transformed outcomes for people with Marfan syndrome. The surgery involves replacing the enlarged portion of the aorta with a synthetic graft. When performed electively before an emergency occurs, this surgery has excellent outcomes. However, emergency surgery for aortic dissection carries significantly higher mortality rates, which is why regular monitoring and timely intervention are so important.
Thanks to improved diagnosis, medical treatment, and surgical techniques, life expectancy for people with Marfan syndrome has increased dramatically. Studies show the median survival has improved from 32 years in untreated patients to nearly normal life expectancy with proper care.
Lifestyle Considerations
Lifestyle modifications play a crucial role in preventing complications. The American Heart Association recommends low to moderate intensity exercise (approximately 4 to 6 metabolic equivalents) for most patients. High intensity competitive sports, contact sports, and activities involving heavy lifting or sudden exertion should generally be avoided as they can increase stress on the aorta. Swimming, walking, and cycling at moderate intensity are typically safe options, but always discuss your specific situation with your cardiologist.
Workplace Accommodations
Under the ADA, employers are required to provide reasonable accommodations for employees with disabilities, including those with Marfan syndrome. Potential accommodations might include modified work schedules, restrictions on heavy lifting or strenuous physical activity, ergonomic workplace adjustments, flexible break times, telecommuting options, and modified job duties to reduce physical demands. The key is open communication with your employer about your needs and limitations.
Conclusion
Marfan syndrome can be a disability, but it does not have to define or limit your life. The key factors determining disability status are the severity of your symptoms, particularly cardiovascular complications, and how they affect your ability to perform daily activities and work. With advances in medical care, including effective medications and life saving surgical techniques, many people with Marfan syndrome now live long, productive lives.
“As a cardiologist, my strongest advice is this: early detection and proactive management are your best tools against disability. Schedule regular cardiac evaluations, take prescribed medications consistently, and learn to recognize warning signs of serious complications. At Atlantic Cardiovascular, our team specializes in comprehensive Marfan syndrome treatment, offering advanced diagnostic imaging, personalized medication management, and expert surgical consultation to help you live your healthiest life.”
Frequently Asked Questions
Is Marfan syndrome always a disability?
No, not everyone with Marfan syndrome is considered disabled. Many people manage the condition effectively with regular monitoring and medication, maintaining active careers and lifestyles. Disability status depends on how severely symptoms affect your ability to perform daily activities and work. Those with serious cardiovascular complications or multiple affected systems are more likely to qualify as disabled.
Can I receive Social Security Disability benefits for Marfan syndrome?
Yes, if your condition is severe enough to prevent you from working. While Marfan syndrome itself is not listed in the Blue Book, you can qualify under related listings for cardiovascular impairments, vision problems, or musculoskeletal disorders. Strong medical documentation is essential. Include all echocardiograms, surgical records, and detailed physician statements describing your limitations.
What heart symptoms should prompt me to seek immediate medical care?
Seek emergency care immediately if you experience sudden, severe chest or back pain (especially a tearing sensation), difficulty breathing, fainting or near fainting, rapid irregular heartbeat, or any sudden change in vision or severe headache. These could indicate aortic dissection or other serious complications that require immediate intervention.
Is Marfan syndrome hereditary, and should my family members be tested?
Yes, Marfan syndrome follows an autosomal dominant inheritance pattern. If you have the condition, each of your children has a 50% chance of inheriting it. First degree relatives (parents, siblings, children) should be evaluated by a physician familiar with Marfan syndrome. Genetic testing and echocardiography can help identify affected family members before complications develop. Genetic counseling is highly recommended for family planning decisions.
What types of exercise are safe for people with Marfan syndrome?
Moderate, low impact activities are generally beneficial and safe. Good options include walking, swimming, light cycling, and gentle yoga. Avoid high intensity workouts, competitive sports, contact sports, heavy weight lifting, and activities that involve sudden bursts of exertion or the Valsalva maneuver (straining while holding your breath). Always discuss your exercise plans with your cardiologist, who can provide personalized recommendations based on your specific cardiovascular status.
References and Resources
For more information about Marfan syndrome and disability, consider these trusted resources:
The Marfan Foundation (marfan.org)
Centers for Disease Control and Prevention (cdc.gov)
National Institutes of Health (nih.gov)
Social Security Administration (ssa.gov)
Job Accommodation Network (askjan.org)
American Heart Association (heart.org)
Medical Disclaimer: This article is for informational purposes only and should not replace professional medical advice, diagnosis, or treatment. Always consult with your healthcare provider regarding your specific situation and treatment options.