Most people think recovery ends when you leave the hospital. It doesn’t. The truth is, what happens next and what you do next will define the rest of your life. Cardiac rehab isn’t just some optional program; it’s the difference between surviving and thriving.
Yet, so many people don’t even know what it is or why it matters. Let’s cut through the noise and talk about the truth no one’s telling you & your heart’s future depends on it.
What is a Cardiac Rehab?
To be honest, when you hear ‘cardiac rehab,’ do you know what it means? If your first thought is exercise classes or lectures, you’re not even scratching the surface. This is about taking back control over your life, your health, and your future.
Cardiac rehab, short for cardiac rehabilitation, is a medically supervised program designed to help people recover, rebuild, and thrive after experiencing a heart-related event or undergoing cardiac procedures. It’s not just about exercise or lectures it’s a comprehensive, personalized plan that supports your heart’s healing and teaches you how to protect it for the future.
Here’s what it typically involves:
- Customized Exercise Plans: Tailored workouts designed to improve your heart health, stamina, and overall fitness under professional supervision.
- Education & Lifestyle Coaching: Guidance on managing risk factors like high cholesterol, blood pressure, or stress, and making heart-friendly choices in diet, exercise, and daily habits.
- Emotional Support: Helping you manage anxiety, depression, or fear that often comes after a heart scare, through counseling or group support.
- Monitoring & Medical Guidance: Regular check-ins with healthcare professionals to track your progress and ensure your recovery is on track.
The Components of Cardiac Rehab
Cardiac rehabilitation is more than just a recovery program—it’s a comprehensive, life-changing approach to improving heart health and preventing future cardiac events. Here are the key components of cardiac rehab:
1. Personalized Medical Evaluation
What It Involves: A thorough assessment of your medical history, current physical condition, and any ongoing health issues.
Why It Matters: This sets the foundation for a customized rehab plan tailored to your unique needs and goals, ensuring safe and effective recovery.
2. Supervised Exercise Training
What It Involves: Structured, heart-safe physical activity such as walking, cycling, or resistance training under the guidance of healthcare professionals.
Why It Matters: Improves cardiovascular fitness, strengthens your heart, and boosts overall stamina, helping you return to daily life with confidence.
3. Lifestyle and Risk Factor Management
What It Involves: Education and coaching on managing key risk factors like high cholesterol, high blood pressure, diabetes, and obesity.
Why It Matters: Helps you adopt heart-healthy habits like better nutrition, regular exercise, and quitting smoking, reducing the risk of another cardiac event.
4. Nutrition Guidance
What It Involves: Advice on heart-healthy eating, including reducing sodium, cutting down on unhealthy fats, and focusing on whole, nutrient-rich foods.
Why It Matters: Proper nutrition supports heart health, lowers cholesterol, and helps maintain a healthy weight.
5. Emotional and Psychological Support
What It Involves: Counseling or support groups to address stress, anxiety, or depression that often follow a heart event.
Why It Matters: Emotional well-being is critical to recovery, as stress and mental health challenges can negatively impact heart health.
7. Regular Monitoring and Progress Tracking
What It Involves: Ongoing medical supervision, including tracking your vitals, fitness levels, and overall progress throughout the program.
Why It Matters: Ensures your rehab plan stays on course and adjustments can be made as needed for optimal results.
8. Long-Term Maintenance Plan
What It Involves: Guidance on continuing heart-healthy habits after the program ends, with strategies for staying active and managing risks.
Why It Matters: Cardiac rehab isn’t a one-time fix—it’s about sustaining a heart-healthy lifestyle for the long haul.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsThe Three Main Phases of Cardiac Rehab
Cardiac rehabilitation is structured into three key phases, each designed to guide you from immediate recovery to long-term heart health.
Phase 1: The Acute or In-Hospital Phase
What It Is:
This phase begins immediately after a heart event, such as a heart attack, surgery, or diagnosis of a cardiac condition, and takes place while you’re still in the hospital.
What Happens:
- Medical professionals monitor your recovery closely.
- Gentle, supervised physical activity starts to improve circulation and prevent complications like blood clots.
- You’ll receive initial education about your condition, medications, and lifestyle changes.
Why It Matters:
This phase focuses on stabilizing your health, preventing further complications, and preparing you for the next stages of recovery.
Phase 2: The Outpatient or Early Recovery Phase
What It Is:
After being discharged, this phase typically lasts 6-12 weeks and involves attending a structured rehab program at a medical center or clinic.
What Happens:
- Supervised exercise sessions tailored to your fitness and health goals.
- Education on managing risk factors like high blood pressure, cholesterol, or stress.
- Counseling to address mental health concerns like anxiety or depression.
Why It Matters:
This phase is the heart of cardiac rehab, helping you regain physical strength, build healthy habits, and rebuild confidence in your ability to live a full life.
Phase 3: The Long-Term Maintenance Phase
What It Is:
This ongoing phase focuses on maintaining the progress you’ve made and integrating heart-healthy habits into your everyday life.
What Happens:
- Continued exercise, either independently or in community-based programs.
- Regular follow-ups with your healthcare team to track your health and make adjustments.
- Long-term lifestyle changes, including a balanced diet, stress management, and medication adherence.
Why It Matters:
The goal of this phase is to prevent future cardiac events and ensure a lasting improvement in your quality of life.
Can You Do Your Cardiac Rehab at Home?
The short answer is yes, you can do cardiac rehab at home—but it depends on your specific situation and requires proper planning and supervision to ensure safety and effectiveness.
Should You Consider Home-Based Rehab?
Home-based rehab can be a safe and effective option for Phase 2 and Phase 3 if:
- Your doctor clears you for independent exercise.
- You have access to the necessary tools, like a wearable heart monitor or virtual consultations.
- You’re committed to following the program diligently.
How Do You Prepare for Cardiac Rehab?
Starting cardiac rehab can feel like stepping into the unknown, but with the right preparation, you can set yourself up for success. Preparation begins with understanding what to expect.
Your healthcare team plays a big role in getting you ready. They’ll conduct evaluations, like a stress test or an electrocardiogram (ECG), to determine how much activity your heart can handle safely.
They might also adjust your medications to ensure your heart is stable before you begin. If you have questions or concerns, this is the time to ask them. Knowing how your rehab will be structured—whether it’s in-person sessions or at home—can ease any anxiety.
It’s also important to prepare physically and practically. Make sure you have comfortable clothing, supportive shoes, and any necessary devices like a fitness tracker. If your sessions are at a facility, plan how you’ll get there and back. For those doing rehab at home, set aside a dedicated, distraction-free space for your activities.
What Would Your Cardiac Rehab Look Like?
Your journey begins with a thorough evaluation by your rehab team, which may include cardiologists, physical therapists, nutritionists, and counselors. They’ll assess your medical history, physical fitness, and emotional state to create a plan just for you.
You’ll also discuss your personal goals. Whether it’s regaining energy, reducing the risk of future cardiac events, or returning to daily activities with confidence, these goals will shape the program.
Physical activity is a core part of cardiac rehab, but it’s far from a generic workout. Your exercises will be tailored to your fitness level and closely monitored to ensure your heart responds well.
This might include:
- Aerobic Exercises: Activities like walking on a treadmill or cycling to improve your cardiovascular health and stamina.
- Strength Training: Gentle resistance exercises to build muscle and support overall body strength.
- Flexibility Work: Stretches or yoga to improve mobility and reduce stiffness.
All exercises are done under the supervision of trained professionals who monitor your vitals and adjust the intensity as needed. As you progress, the exercises may become more challenging to keep pushing your heart toward optimal health.
During your sessions, you’ll learn about factors that influence heart health, like diet, stress, sleep, and smoking. You’ll work with dietitians to understand what a heart-healthy diet looks like. This often involves learning how to incorporate more whole foods, reduce sodium, and balance your nutrients effectively. If you’re a smoker, smoking cessation support may be part of your plan.
Heart events often bring emotional challenges like anxiety, depression, or fear of recurrence. Your cardiac rehab may include counseling sessions, either one-on-one or in a group, to address these feelings. You’ll learn strategies to cope with stress and regain confidence in your body and its ability to recover.
What Would Be the Duration of Cardiac Rehab?
The typical duration of a cardiac rehab program is 6 to 12 weeks for structured sessions, followed by a lifetime commitment to maintaining heart health. However, this timeline can vary based on your health status and recovery goals. Regardless of how long it takes, the journey through cardiac rehab is one of the most impactful investments you can make in your heart’s future.
What Are the Success Rates of Cardiac Rehab?
Cardiac rehab is highly effective in improving heart health and reducing future risks. Studies show it can lower cardiovascular mortality by 26-31% and reduce overall mortality by up to 25%. The likelihood of another heart attack or cardiac event drops by 20-30%, and hospital readmission rates decrease by 30%.
Participants typically see a 15-25% improvement in cardiovascular fitness and significant benefits in emotional well-being, with anxiety and depression levels reduced by 20-40%. Lifestyle changes like increased physical activity, better diet, and smoking cessation are often sustained long-term. However, success depends on participation, as only 20-30% of eligible patients enroll in cardiac rehab.
What Are the Best Ways to Choose a Cardiac Rehab Program?
Choosing the right cardiac rehab program is a critical step in your recovery journey. A well-suited program ensures your safety, meets your needs, and sets you up for long-term success. Here’s how to make the best choice:
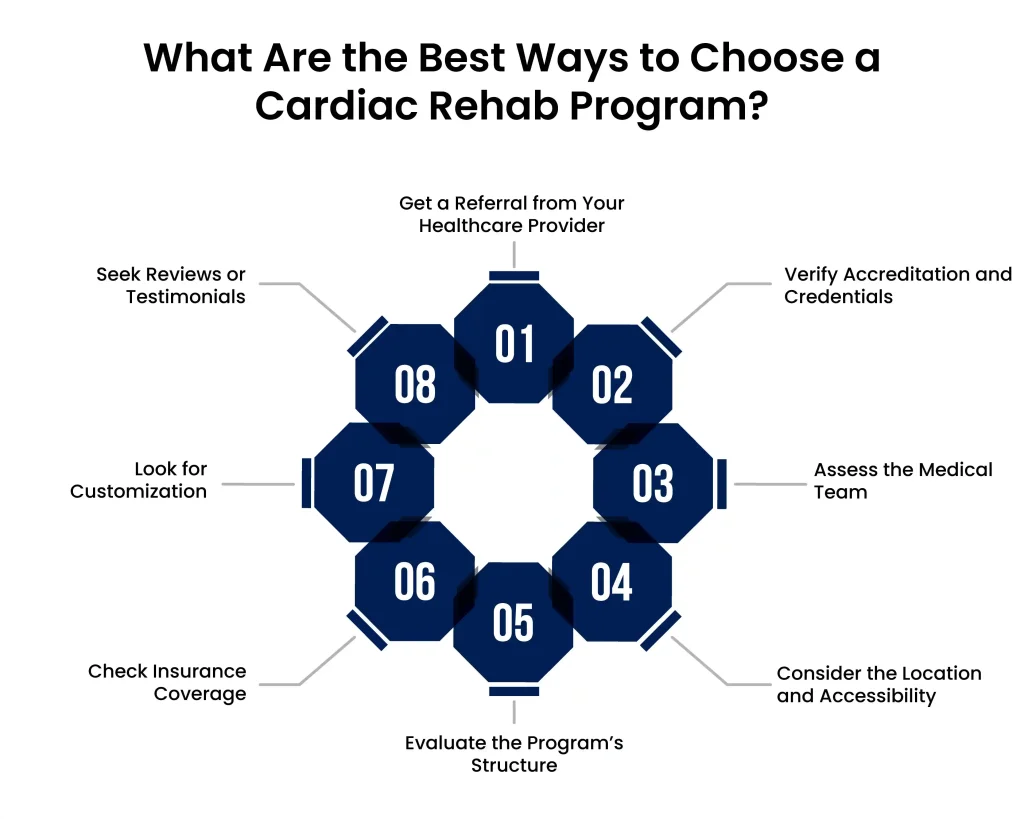
1. Get a Referral from Your Healthcare Provider
Your doctor or cardiologist will recommend a program that suits your medical condition and recovery goals. Start by asking them for options they trust and have experience with.
2. Verify Accreditation and Credentials
Look for programs that are accredited by reputable organizations, such as the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR). Accreditation ensures the program meets high standards of care.
3. Assess the Medical Team
Ensure the program is run by qualified professionals, including cardiologists, nurses, physical therapists, and dietitians. A multidisciplinary team is essential for comprehensive care.
4. Consider the Location and Accessibility
Choose a program that is conveniently located or offers flexible options, such as virtual or home-based rehab, to ensure you can attend consistently.
Prevent heart problems before they start – Schedule a preventive checkup
Contact Us5. Evaluate the Program’s Structure
Ask about the program’s components, including supervised exercise sessions, educational materials, emotional support, and long-term follow-up. A well-rounded program should address all aspects of heart health.
6. Check Insurance Coverage
Confirm that the program is covered by your insurance or inquire about out-of-pocket costs. Many programs offer financial assistance if needed.
7. Look for Customization
Ensure the program tailors its approach to your specific condition, fitness level, and recovery goals. A personalized plan is key to effective rehabilitation.
8. Seek Reviews or Testimonials
Ask previous participants about their experiences or look for reviews online. Positive feedback can indicate a program’s success and patient satisfaction.
A Note From Atlantic Cardiovascular Cardiologist
Your heart has been through a lot, and now it’s time to give it the care it deserves Cardiac rehab is a step closer in recovery. Whether you’re recovering from a heart attack, surgery, or managing a chronic condition, this program is your opportunity to take charge of your future.
At Atlantic Cardiovascular, we’ve seen firsthand how cardiac rehab transforms lives. Patients who commit to the program not only regain physical strength but also discover renewed hope and resilience. It’s about more than exercise; it’s about giving your heart and your life a second chance.