Approximately 1.28 billion adults worldwide aged 30–79 have hypertension, a condition that quietly undermines health with potentially severe consequences. Among these, a significant number still grapple with an understanding of what hypertension really entails—particularly the diastolic measurement, which often remains a silent concern.
Diastolic blood pressure, the bottom number in a blood pressure reading, reflects the pressure in your arteries when the heart is resting between beats. While many are familiar with the term ‘high blood pressure’, few are aware that the causes and implications of a high diastolic reading can be distinctly different and equally serious.
In this blog, we will delve into the various factors that can lead to elevated diastolic blood pressure, offering clarity and insight to help you better manage or prevent this hidden health risk.
What is Diastolic Blood Pressure?
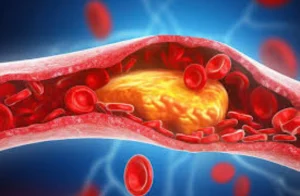
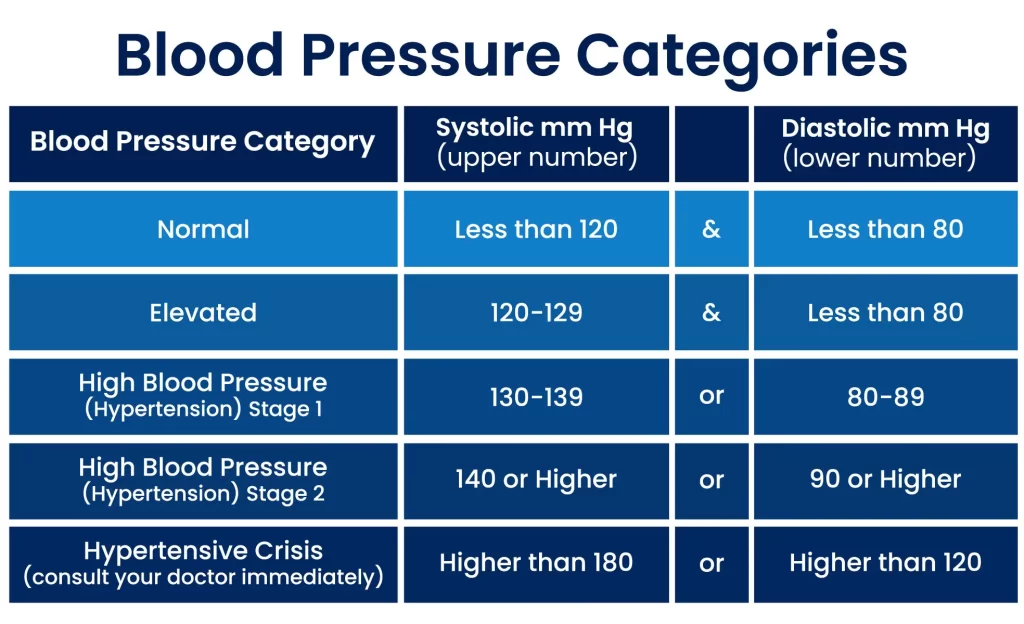
Doctors usually measure blood pressure based on two readings: one is called systolic, and the other is called diastolic. Systolic pressure, the top number, indicates how much pressure your blood is exerting against your artery walls when the heart beats. Diastolic pressure, the bottom number, measures the pressure in the arteries when the heart is resting between beats. It’s a critical indicator of your overall vascular health.
While normal diastolic blood pressure is typically lower than the systolic, it is equally important in assessing the risk of heart disease and stroke. A normal diastolic reading is usually between 60 and 80 mmHg.
When these numbers climb consistently above 80, it is considered elevated or high diastolic blood pressure, also known as diastolic hypertension. Understanding what a normal diastolic reading looks like and recognizing when it deviates from this norm can be crucial for early detection and management of potential health issues.
What Causes Your Diastolic Blood Pressure To Be High?
When it comes to managing and diagnosing hypertension, doctors focus on two key measurements: systolic and diastolic blood pressure. However, there are cases where the systolic blood pressure (the top number) remains within the normal range, but there is a noticeable rise in the diastolic blood pressure (the bottom number). This condition is known as isolated diastolic hypertension.
Some of the lifestyle factors that can cause high diastolic Pressure Include:
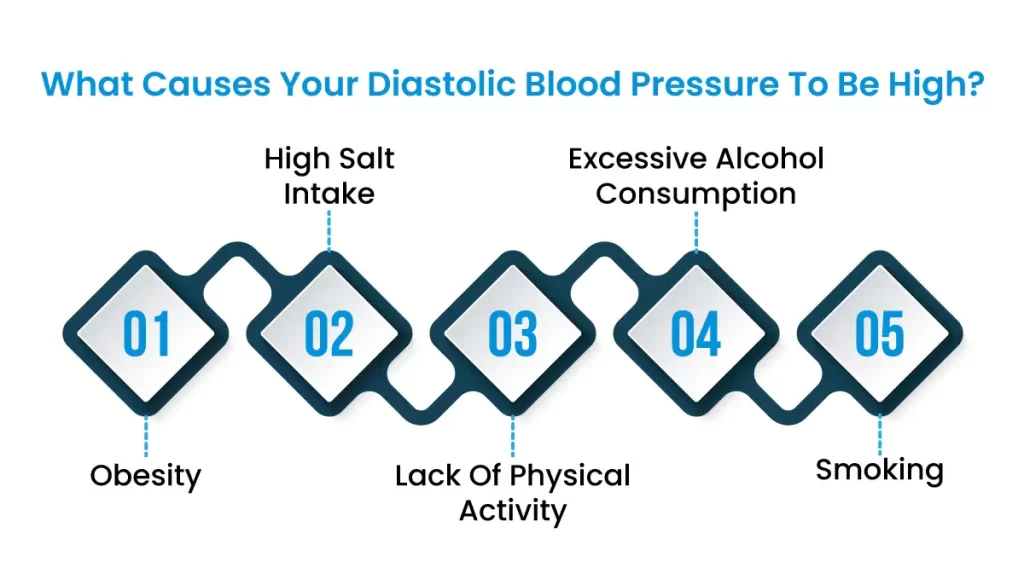
Obesity
Obesity is a significant health concern globally and plays a crucial role in influencing diastolic blood pressure. In individuals with obesity, excess body fat leads to several physiological changes that can increase diastolic pressure. One of the primary mechanisms involves the strain that excess weight places on the heart and blood vessels.
When you have excess body fat, your heart needs to work harder to pump blood throughout a larger network of blood vessels. This increased blood volume puts extra strain on the arteries, raising the pressure even when your heart is at rest.
Obese individuals often have imbalances in hormones like leptin and insulin, which can contribute to blood vessel constriction and fluid retention, further raising blood pressure
Obesity triggers chronic inflammation in the body. This damages blood vessels and promotes stiffness, increasing diastolic pressure.
High Salt Intake
High salt intake is another significant factor that contributes to high diastolic blood pressure. Salt, or sodium chloride, is essential for body functions, but when consumed in excess, it can lead to several adverse health effects, particularly in terms of blood pressure.
Salt (sodium chloride) attracts and holds onto water. A high salt diet causes your body to retain extra fluid, increasing blood volume. This puts more pressure on your artery walls, raising your blood pressure (both systolic and diastolic).
Your kidneys are crucial for regulating blood pressure. They filter excess water and sodium from your blood. Too much salt can overburden your kidneys, making them less efficient leading to fluid buildup and higher pressure.
Over time, a consistently high salt intake can damage and stiffen your blood vessels. This makes it harder for blood to flow smoothly, increasing the resting pressure on your arteries (diastolic).
High salt consumption can disrupt the balance of hormones involved in blood pressure regulation, making blood vessels more likely to constrict, further elevating pressure.
Lack Of Physical Activity
Just like any muscle, the heart becomes stronger and more efficient with regular exercise. A sedentary lifestyle leads to a weaker heart that has to work harder to circulate blood. While it might pump harder initially, this increases your systolic BP, but over time, even the resting pressure in your arteries (diastolic) starts to rise.
A study found that sedentary behavior was linked to higher diastolic blood pressure, even independently of traditional risk factors like obesity.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsExcessive alcohol consumption
Even short-term, alcohol temporarily constricts blood vessels and increases the force of your heartbeats. With chronic excessive use, this can lead to longer-lasting blood vessel stiffness and higher pressure, including higher diastolic readings.
Alcohol interferes with the production and function of hormones that regulate blood pressure, like those involved in fluid balance. This imbalance can lead to fluid retention and increased resting pressure.
Those drinking 6-8 drinks per day had significantly higher systolic and diastolic readings compared to non-drinkers.
Smoking
The nicotine in cigarettes triggers the release of adrenaline and other chemicals that temporarily constrict blood vessels and increase heart rate. Each cigarette causes a sharp spike in both systolic and diastolic blood pressure.
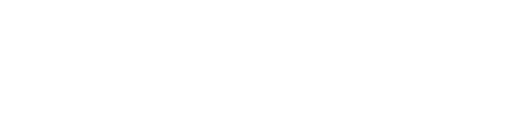
Smoking damages the lining of your arteries, promoting inflammation and the buildup of plaque. This stiffening and narrowing of the arteries makes it harder for blood to flow, leading to an increased resting pressure (diastolic) even between cigarettes.
Numerous studies show an immediate rise in both systolic and diastolic blood pressure for up to 30 minutes after smoking a cigarette.
What Does It Mean If My Diastolic Blood Pressure Is High?
A high number means your heart is working harder than it should, even at rest. Consistently high diastolic blood pressure puts you at increased risk of:
- Heart disease
- Stroke
- Kidney problems
- Vision issues
High diastolic pressure isn’t a disease but a sign that something is affecting your cardiovascular health. If you have high diastolic readings, it’s crucial to see your doctor. They can help identify the cause, recommend lifestyle changes, and potentially prescribe medication to lower your blood pressure and protect your health.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsWhat Measures You Should Take To Lower Your Diastolic Blood Pressure?
Lowering your diastolic blood pressure is not only essential for your cardiovascular health but can also enhance your overall quality of life. Here are detailed and practical steps you can take to manage and reduce your diastolic blood pressure effectively:
Using DASH Diet
The DASH diet (Dietary Approaches to Stop Hypertension) is specifically designed to combat high blood pressure.
- Prioritize fruits, vegetables, whole grains, and lean proteins. These foods are packed with nutrients that support healthy blood vessels and overall well-being.
- Limit saturated and trans fats: These unhealthy fats can promote inflammation and increase blood pressure.
- Cut back on salt: Aim for no more than 2300 mg of sodium per day, or ideally under 1500mg. Excess salt causes your body to retain water, increasing blood volume and pressure.
- Boost potassium: This mineral helps counteract sodium. Find it in foods like bananas, spinach, beans, and potatoes.
Regular Exercise
- Aim for at least 150 minutes of moderate-intensity exercise per week (30 minutes most days). This can include brisk walking, biking, swimming, or dancing.
- Even small increases in physical activity count! Build up your endurance gradually if needed.
- Resistance training (strength exercises) a few times a week can complement your cardio routine.
Healthy Weight Management
Even modest weight loss (5-10% of body weight) can significantly lower blood pressure.
Managing Stress
- Chronic stress can trigger your nervous system and raise blood pressure.
- Explore stress-reducing techniques like yoga, meditation, deep breathing, or spending time in nature.
- Consider talking to a therapist to develop coping mechanisms.
Limit Alcohol Consumption
- Excessive alcohol raises blood pressure acutely and in the long term.
- Stick to the recommended guidelines: one drink per day for women or a maximum of two for men.
Quit Smoking
- Smoking damages blood vessels and puts a tremendous burden on your heart.
- Quitting offers benefits for your blood pressure and overall health at any age.
When Medications May Be Necessary
If lifestyle changes alone aren’t enough, your doctor may recommend medications. Some common types include:
- Diuretics: Often called “water pills”, these help your body eliminate excess fluid and salt, reducing blood volume.
- ACE inhibitors or Angiotensin II Receptor Blockers (ARBs): These protect the integrity of your blood vessels and decrease their resistance to blood flow.
- Calcium channel blockers: These help relax and widen blood vessels.
The Low Down
Effectively managing high diastolic blood pressure is crucial for your heart health and overall well-being. By adopting lifestyle changes such as improved diet, increased physical activity, and stress reduction, along with adherence to medical advice and medications if necessary, you can significantly lower your risk of cardiovascular complications.
Regular monitoring and consultations with your healthcare provider are essential to tailor your treatment plan effectively. For expert guidance and personalized care in managing hypertension, consider consulting a cardiologist at Atlantic Cardiovascular. Remember, taking proactive steps toward managing your blood pressure not only safeguards your health but also enhances your quality of life. Start today, and make a lasting commitment to your heart health.