Heart failure. It’s a scary phrase, right? But did you know that there are actually four distinct stages of heart failure, and knowing which one you’re in can make all the difference in your treatment and outlook?
Whether you’re already living with heart problems or simply want to be proactive about your health, this guide will give you the knowledge you need to take charge of your heart health.
Understanding Congestive Heart Failure
Let’s get right to the heart of the matter. Congestive heart failure, often simply called heart failure, doesn’t mean your heart has completely stopped. It means your heart isn’t pumping blood as effectively as it should.
Think of it like a pump struggling to keep up with the demand. This can lead to fluid buildup in your body, especially in your lungs and legs, causing a whole host of uncomfortable symptoms.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsWhat are the 4 Stages of Congestive Heart Failure?
In an effort to standardize the assessment and treatment of heart failure, the American College of Cardiology (ACC) and the American Heart Association (AHA) jointly developed a staging system that categorizes the progression of the disease.
This classification system offers a valuable framework for both healthcare providers and patients, aiding in risk assessment, treatment planning, and disease management.
The ACC/AHA stages are progressive, meaning they represent the gradual worsening of the condition over time. Each stage is characterized by specific symptoms, levels of heart dysfunction (how well the heart is pumping), functional limitations (what activities become difficult), and the overall impact on the patient’s quality of life.
This structured approach allows for a more personalized and tailored treatment plan, as the appropriate interventions may vary significantly depending on the stage of heart failure.
- Stage A: At Risk
- Stage B: Pre-Heart Failure
- Stage C: Heart Failure
- Stage D: Advanced Heart Failure
Stage A: At Risk for Congestive Heart Failure
Stage A is the earliest phase in the development of heart failure, and it’s characterized by the presence of risk factors but no noticeable symptoms or structural changes to the heart. In this stage, individuals are considered to be at high risk of developing heart failure in the future due to underlying conditions or lifestyle choices that put a strain on their cardiovascular system.
These risk factors often include:

- High blood pressure (hypertension): The persistent strain of high blood pressure can weaken the heart muscle over time.
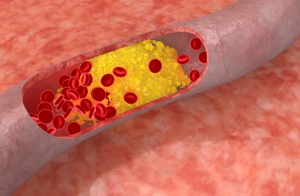
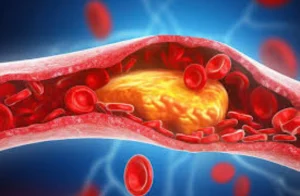
- Coronary artery disease: Narrowed arteries can restrict blood flow to the heart, depriving it of oxygen and nutrients.
- Diabetes: High blood sugar levels can damage blood vessels and nerves, affecting the heart’s function.
- Obesity: Excess weight puts additional strain on the heart and can contribute to other risk factors like high blood pressure and diabetes.
- Family history of heart disease: Genetics can play a role in predisposing individuals to heart problems.
- History of alcohol or substance abuse: These substances can directly damage the heart muscle.
While there are no outward signs of heart failure in stage A, it’s crucial to recognize and address these risk factors early on.
Stage A: Life Expectancy and Progression
A study published in Circulation: Cardiovascular Quality and Outcomes followed 413 patients with stage A heart failure over four years and found that 35% progressed to stages B or C within that timeframe. This underscores the importance of early identification and intervention for risk factors.
Life expectancy in stage A varies greatly, depending on age, overall health, and any coexisting medical conditions. Specific survival rates for stage A aren’t typically reported, but a 2007 study indicated a 97% five-year survival rate for individuals with stage A heart failure.
Stage A Treatment
The primary goal of treatment in Stage A heart failure is to prevent the progression to more advanced stages. This involves a multi-faceted approach that focuses on addressing underlying risk factors and promoting heart-healthy behaviors.
Diet: Adopting a heart-healthy diet, rich in fruits, vegetables, whole grains, and lean proteins, while limiting saturated fats, trans fats, cholesterol, and sodium can significantly improve cardiovascular health.
Exercise: Regular physical activity, such as brisk walking, swimming, or cycling, for at least 30 minutes most days of the week strengthens the heart and improves overall fitness.
Weight Management: Maintaining a healthy weight reduces strain on the heart and helps control blood pressure and cholesterol levels.
Smoking Cessation: Quitting smoking is essential for heart health, as smoking significantly damages blood vessels and increases the risk of heart disease.
Alcohol Moderation: Excessive alcohol consumption can weaken the heart muscle. Men should limit themselves to no more than two drinks per day, and women should have no more than one.
Stage B: Pre-Heart Failure
Stage B marks the transition from “at risk” to “pre-heart failure.” While still not experiencing any overt symptoms, individuals in this stage have developed structural changes in their heart. This typically means the heart’s main pumping chamber, the left ventricle, has become either weakened (reduced ejection fraction) or stiff (preserved ejection fraction), compromising its ability to pump blood efficiently.
Key Characteristics of Stage B:
- Structural Heart Changes: Imaging tests like echocardiograms or cardiac MRIs may reveal enlargement or thickening of the left ventricle, indicating the heart is working harder to compensate for its reduced pumping capacity.
- No Noticeable Symptoms: Despite the structural changes, most people in stage B don’t experience any noticeable symptoms. This highlights the importance of regular checkups and screening tests, especially for those with known risk factors.
Stage B: Life Expectancy and Progression
Stage B heart failure, while asymptomatic, is not without the risk of progression. Over time, the underlying structural changes in the heart can worsen, potentially leading to symptomatic heart failure (stages C and D). A study published in Circulation: Cardiovascular Quality and Outcomes followed individuals with preclinical heart failure, including those in stage B, and found that 6% progressed to symptomatic heart failure over a four-year period.
In general, the long-term outlook for stage B heart failure can be relatively positive. A 2007 study reported a 95.7% five-year survival rate for individuals in this stage.
Individuals with stage B heart failure due to reduced ejection fraction (HFrEF), where the heart’s pumping ability is weakened, face a higher risk of progression to symptomatic heart failure and may experience lower survival rates compared to those with preserved ejection fraction (HFpEF), where the heart muscle is stiff but the pumping ability is relatively normal.
Stage B Treatment
The goal of treatment in Stage B heart failure is twofold: to prevent the progression to symptomatic heart failure and to manage any underlying conditions that are contributing to heart dysfunction. The same heart-healthy lifestyle changes recommended for Stage A remain crucial in Stage B.
Stage B may require medications to manage heart function and prevent further deterioration.
- Angiotensin Receptor-Neprilysin Inhibitors (ARNIs): This class of drugs combines the benefits of ACE inhibitors and neprilysin inhibitors, offering superior protection against heart failure progression compared to ACE inhibitors alone.
- Beta-blockers: These medications slow the heart rate and lower blood pressure, reducing the workload on the heart and improving its function over time.
- Aldosterone Antagonists: These drugs help manage fluid retention, which can worsen heart failure symptoms and may also have protective effects on the heart.
- SGLT2 Inhibitors: Originally developed for diabetes, these drugs have shown promising benefits in reducing hospitalization and death in people with heart failure.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsStage C: Heart Failure
Stage C marks a pivotal point in the progression of heart failure, as this is when the condition becomes symptomatic. The structural changes that began in earlier stages have now significantly impacted the heart’s ability to pump blood effectively, leading to a variety of noticeable symptoms that can range from mild to severe.
Key Characteristics of Stage C:
Individuals in Stage C experience a range of symptoms due to fluid buildup and inadequate blood flow. These symptoms can include:
- Shortness of breath: Difficulty breathing, especially during exertion or when lying down.
- Fatigue: Feeling tired and weak, even with minimal activity.
- Swelling (edema): Fluid buildup in the legs, ankles, feet, or abdomen.
- Rapid or irregular heartbeat: Palpitations or a feeling of a racing heart.
- Persistent cough or wheezing: Often worse at night or when lying down.
- Reduced ability to exercise: Difficulty performing activities that were previously easy.
Stage C: Life Expectancy and Progression
The trajectory of Stage C heart failure can be quite variable. For some individuals, the condition remains stable for many years with proper management, while for others, it can progress to the advanced stage D.
A study published in the Journal of the American College of Cardiology found that, over a three-year period, 4.5% of individuals with stage C heart failure and reduced ejection fraction (HFrEF) progressed to stage D.
The overall five-year survival rate for stage C heart failure is approximately 75%, meaning that 3 out of 4 individuals are alive after five years.
Stage C Treatment
Several medications are commonly used in stage C heart failure, in addition to those used in earlier stages:
Diuretics: These medications help eliminate excess fluid from the body, reducing swelling and easing breathing difficulties.
Vasodilators: These drugs relax blood vessels, making it easier for the heart to pump blood and lowering blood pressure.
Inotropes: These medications help strengthen the heart’s contractions, improving its pumping ability, but are typically reserved for short-term use in severe cases.
Aldosterone Antagonists: These drugs help manage fluid retention and may also have protective effects on the heart.
SGLT2 Inhibitors: Originally developed for diabetes, these drugs have shown promising benefits in reducing hospitalization and death in people with heart failure.
Device Therapy:
In some cases, implantable devices may be recommended:
- Cardiac Resynchronization Therapy (CRT): This involves implanting a pacemaker that helps coordinate the heart’s contractions, improving its pumping efficiency.
- Implantable Cardioverter Defibrillator (ICD): This device monitors heart rhythm and can deliver a shock to restore normal rhythm if a life-threatening arrhythmia occurs.
Stage D: Advanced Heart Failure
Stage D is the most advanced stage of heart failure, characterized by severe symptoms that persist despite optimal medical therapy. At this stage, the heart’s pumping ability is significantly impaired, leading to marked limitations in daily activities and a reduced quality of life.
Stage D: Life Expectancy
Stage D heart failure carries a significantly poorer prognosis compared to earlier stages. The five-year survival rate for individuals in this stage is estimated to be around 20%, meaning only 1 in 5 individuals survive for five years after reaching this advanced stage.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsStage D Treatment
The medications used in earlier stages often continue in stage D, but dosages may be adjusted or additional medications added to manage specific symptoms. These may include:
- Diuretics: To manage fluid retention and reduce swelling.
- Vasodilators: To relax blood vessels and improve blood flow.
- Inotropes: To strengthen the heart’s contractions and improve cardiac output.
- Other Medications: Depending on individual needs, other medications may be prescribed to manage specific symptoms, such as pain, anxiety, or depression.
Advanced Therapies:
For some individuals in stage D, advanced therapies may be considered to improve quality of life and prolong survival:
- Continuous Intravenous Inotropes: For individuals with severe symptoms, continuous infusion of inotropes may be necessary to maintain adequate blood flow and organ function.
- Mechanical Circulatory Support (MCS): These devices, such as ventricular assist devices (VADs) or total artificial hearts (TAHs), can help pump blood and support the failing heart. VADs are often used as a bridge to transplant, while TAHs may be considered for individuals who are not transplant candidates.
- Heart Transplant: For select patients, a heart transplant may be the only option for long-term survival. However, not all individuals are eligible for transplantation due to age, other medical conditions, or organ availability.
Palliative Care:
Palliative care plays a crucial role in stage D heart failure, focusing on relieving symptoms, managing pain, and providing emotional and spiritual support to both patients and their families. Palliative care can be initiated alongside other treatments and can help individuals live as comfortably as possible while managing their condition.
End-of-Life Care:
In some cases, when the focus shifts from curative to comfort care, hospice may be considered to provide compassionate end-of-life support.
Final Words
Heart failure is a serious but manageable condition. Understanding the four stages—from “at risk” to “advanced heart failure”—empowers you to take proactive steps in protecting your heart health. Early intervention, lifestyle changes, and appropriate medical treatment can significantly impact your well-being and outlook.
Whether you’re in stage A, focused on prevention, or overcoming the challenges of stage D, knowledge is your most powerful tool. Talk openly with your doctor, prioritize heart-healthy habits, and explore all available treatment options. Remember, even in the face of advanced heart failure, there are ways to improve your quality of life and find comfort and support.