Your heart’s job is simple: pump blood to keep your body working. But when the heart can’t pump as well as it should, it’s called heart failure. This doesn’t mean the heart has stopped, but it does mean it’s struggling to meet the body’s needs.
There are two main types of heart failure: systolic and diastolic. Systolic heart failure happens when the heart is weak and can’t pump blood out effectively. Diastolic heart failure happens when the heart is stiff and can’t fill with blood properly.
In this blog, we’ll explain what causes these problems, what symptoms you might notice, and how doctors treat them.
What is Meant By Systolic Heart Failure?
Systolic heart failure, also called heart failure with reduced ejection fraction (HFrEF), occurs when the heart’s main pumping chamber (the left ventricle) can’t contract with enough force to push blood out to the rest of the body. This means less oxygen-rich blood is delivered to meet the body’s needs.
In simple terms, the heart’s ability to squeeze or pump blood is weakened. Think of it like a weak pump that can’t generate enough pressure to move fluid efficiently. This condition can result from various causes, including damage to the heart muscle, which reduces its strength.
Symptoms of Systolic Heart Failure
When the heart can’t pump blood effectively, you may experience symptoms like:
- Shortness of breath (especially during physical activity or when lying down).
- Fatigue and weakness due to reduced oxygen delivery.
- Swelling in the legs, ankles, or feet caused by fluid buildup.
- Rapid or irregular heartbeat.
- Coughing or wheezing, sometimes with pink, frothy mucus.
How Do Doctors Determine Ejection Fractions?
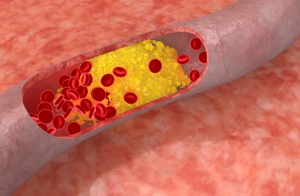
Diagnosing systolic heart failure often starts with understanding the heart’s pumping ability, specifically its ejection fraction (EF). Ejection fraction is a measurement that shows how much blood the heart pumps out of the left ventricle with each beat. It’s expressed as a percentage. In a healthy heart, the ejection fraction is typically between 50% and 70%. In systolic heart failure, the ejection fraction is reduced, often below 40%.
1. Echocardiogram (Echo)
2. Cardiac MRI
3. Nuclear Heart Scan (MUGA Scan)
4. Cardiac Catheterization (Angiography)
5. Other Imaging Tests
Why Ejection Fraction Matters in Diagnosis
A low ejection fraction confirms reduced pumping ability, the hallmark of systolic heart failure. By combining EF results with other diagnostic tests, doctors can pinpoint the condition’s severity and underlying causes, helping them create a personalized treatment plan.
Early and accurate diagnosis makes it possible to manage symptoms, slow disease progression, and improve quality of life. If you’re experiencing symptoms like shortness of breath, fatigue, or swelling, seeking medical evaluation is a critical first step.
What is Meant By Diastolic Heart Failure?
Diastolic heart failure, also called heart failure with preserved ejection fraction (HFpEF), occurs when the heart’s left ventricle becomes stiff or less flexible, making it difficult for the heart to fill properly with blood between beats.
Even though the heart’s pumping strength (ejection fraction) may appear normal, the reduced filling capacity limits the amount of blood available to be pumped out, causing similar symptoms to other forms of heart failure.
In simpler terms, diastolic heart failure is a problem with the heart’s relaxation phase. While systolic heart failure is about the heart struggling to pump, diastolic heart failure is about the heart struggling to relax.
Are the Symptoms of Diastolic Heart Failure Different from Systolic Heart Failure?
The symptoms of diastolic heart failure (HFpEF) and systolic heart failure (HFrEF) are often quite similar because both types lead to the same overall issue: the heart’s inability to meet the body’s demand for blood and oxygen. However, there are subtle differences in how these conditions develop and present themselves.
Why Do the Symptoms Overlap?
Despite the differences in underlying mechanisms—stiffness in diastolic failure versus weak pumping in systolic failure—both result in similar downstream effects. The body’s tissues don’t get enough oxygen-rich blood, and fluid backs up in the lungs and other parts of the body.
Treatment Options for Systolic and Diastolic Heart Failure
Managing heart failure, whether systolic or diastolic, requires a tailored approach based on the underlying cause, severity, and the patient’s overall health. While both conditions share some common treatment principles, their management strategies differ due to the distinct nature of the heart dysfunction in each type.
Treatment for Systolic Heart Failure (HFrEF)
Systolic heart failure, or heart failure with reduced ejection fraction, focuses on improving the heart’s ability to pump blood. The main goals are to reduce symptoms, prevent complications, and enhance quality of life.
1. Medications
Medications play a critical role in systolic heart failure by targeting the weakened heart muscle and addressing contributing factors:
- ACE Inhibitors or ARBs: These relax blood vessels, lower blood pressure, and reduce the strain on the heart. Examples include lisinopril (ACE inhibitor) and losartan (ARB).
- Beta-Blockers: These slow the heart rate and reduce blood pressure, helping the heart pump more efficiently. Examples include carvedilol and metoprolol.
- Aldosterone Antagonists: These diuretics (like spironolactone) help reduce fluid buildup and protect the heart from further damage.
- ARNIs (Angiotensin Receptor-Neprilysin Inhibitors): A newer class of medications (e.g., sacubitril/valsartan) that combines the benefits of ARBs with additional heart protection.
- Diuretics: Help relieve fluid buildup in the lungs and other parts of the body, easing symptoms like swelling and shortness of breath.
- Digoxin: Improves the heart’s pumping ability and controls heart rate in some cases.
2. Lifestyle Modifications
Patients are encouraged to adopt heart-healthy habits, including:
- Low-sodium diet: Reduces fluid retention.
- Regular physical activity: Tailored exercises improve cardiovascular strength without overstraining the heart.
- Quitting smoking and limiting alcohol: Prevents further damage to the heart.
- Weight management: Helps reduce the heart’s workload.
3. Medical Devices and Procedures
In more severe cases, additional interventions may be necessary:
- Implantable Cardioverter-Defibrillators (ICDs): Monitor heart rhythms and deliver shocks to correct dangerous arrhythmias.
- Cardiac Resynchronization Therapy (CRT): Improves coordination between the heart’s chambers, enhancing pumping efficiency.
- Left Ventricular Assist Devices (LVADs): A mechanical pump that helps the heart in end-stage heart failure.
- Heart Transplant: Considered for patients with severe, unmanageable heart failure.
Treatment for Diastolic Heart Failure (HFpEF)
Diastolic heart failure, or heart failure with preserved ejection fraction, focuses on improving the heart’s ability to relax and fill with blood. The primary goal is managing symptoms and underlying conditions that contribute to stiffness in the heart muscle.
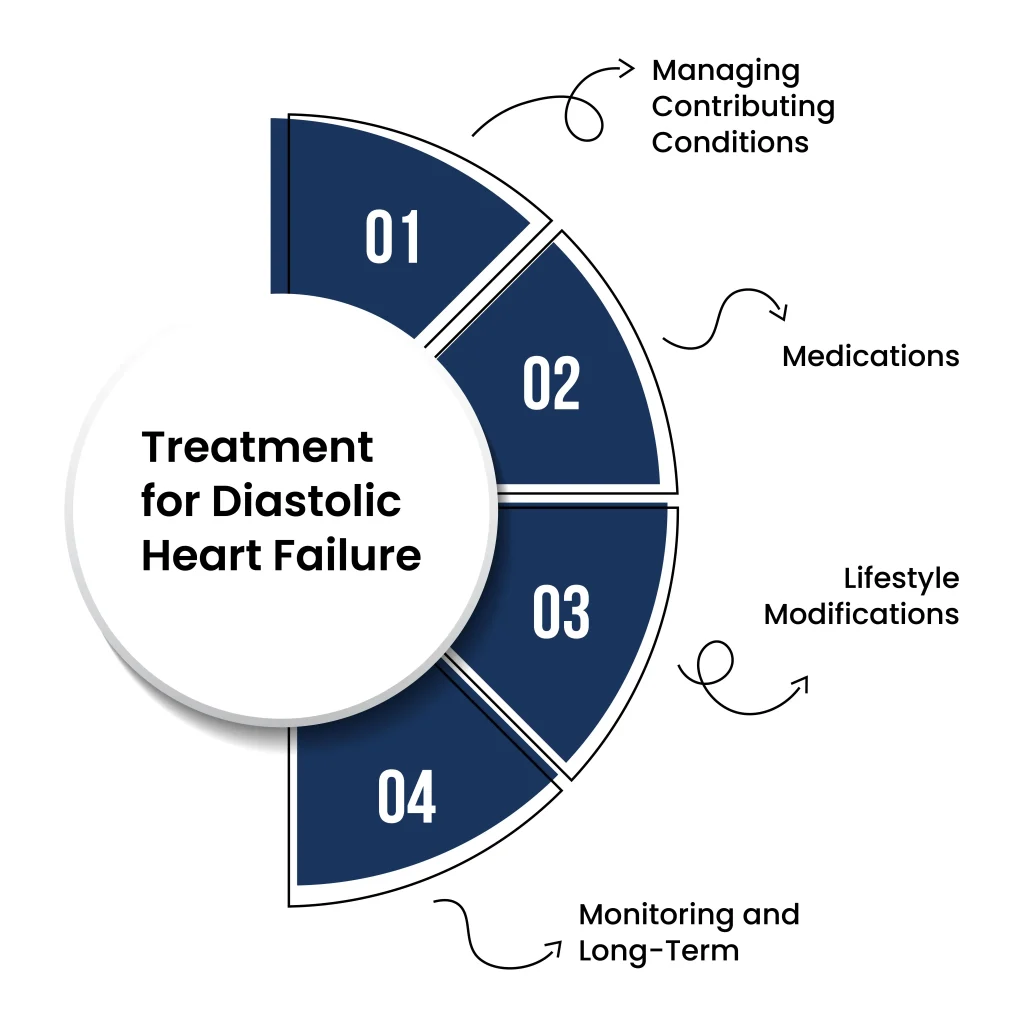
1. Managing Contributing Conditions
The cornerstone of treatment for diastolic heart failure is controlling the underlying conditions that worsen stiffness:
- High Blood Pressure (Hypertension): Aggressive blood pressure management using ACE inhibitors, ARBs, beta-blockers, or calcium channel blockers is crucial to reduce strain on the heart.
- Diabetes Control: Maintaining optimal blood sugar levels prevents further damage to blood vessels and the heart muscle.
- Obesity Management: Weight loss can improve symptoms and reduce the workload on the heart.
2. Medications
Unlike systolic heart failure, there are fewer medications specifically approved for diastolic heart failure. However, certain drugs are used to manage symptoms and contributing factors:
- Diuretics: Help relieve fluid retention and reduce symptoms like swelling and shortness of breath.
- Mineralocorticoid Receptor Antagonists (e.g., spironolactone): May offer benefits in reducing heart stiffness in some patients.
- Beta-Blockers and Calcium Channel Blockers: These drugs improve heart relaxation and slow the heart rate, allowing more time for the heart to fill with blood.
3. Lifestyle Modifications
Similar to systolic heart failure, lifestyle changes are essential for managing diastolic heart failure:
- Low-sodium diet and fluid restriction: Help prevent fluid overload.
- Regular, moderate exercise: Improves cardiovascular fitness and reduces symptoms.
- Stress management: High stress can worsen symptoms by increasing blood pressure and heart rate.
4. Monitoring and Long-Term Care
- Regular follow-ups with a cardiologist are critical to adjust treatments as needed.
- Monitoring for worsening symptoms, like increased shortness of breath or swelling, helps catch complications early.
Key Differences in Treatment Approaches
- In systolic heart failure, the focus is on improving the heart’s pumping ability using medications and devices.
- In diastolic heart failure, the primary aim is managing contributing conditions and improving the heart’s relaxation phase.
Final Words
Heart failure, whether systolic or diastolic, is a serious condition that requires careful management and a personalized approach. Understanding the differences between these two types helps in recognizing symptoms, seeking timely medical attention, and adhering to the right treatment plan.
With the right combination of medications, lifestyle changes, and medical care, it’s possible to manage symptoms, improve quality of life, and prevent complications. Remember, early intervention is key—if you or a loved one experiences signs of heart failure, consult a healthcare provider without delay. Your heart health matters!