The connection between kidney health and blood pressure is often underestimated, but renal hypertension is a powerful reminder of how intertwined they are. This condition develops quietly, with symptoms that can be difficult to detect without proper awareness. In this guide, we’ll explore the warning signs of renal hypertension and help you decide when it’s time to act.
What is Renal Hypertension?
Renal Hypertension also referred to as renovascular hypertension—is a type of high blood pressure that results from narrowed or blocked arteries that supply blood to the kidneys. The condition is primarily caused by a decrease in blood flow to the kidneys, which triggers the body to respond by increasing blood pressure to compensate for the reduced perfusion.
How It Happens
The kidneys play a central role in regulating blood pressure by controlling the balance of fluid and salt in the body. When the blood flow to the kidneys is compromised due to narrowing (stenosis) or blockage in the renal arteries, the kidneys interpret it as low blood pressure. In response, they release hormones like renin, which activates a chain reaction (the renin-angiotensin-aldosterone system or RAAS) that leads to:
- Vasoconstriction: Narrowing of blood vessels.
- Fluid Retention: Increased salt and water retention to boost blood volume.
This results in persistently high blood pressure, often resistant to conventional treatments.
What Are the Main Causes Behind Renal Hypertension?
A significant majority of renal hypertension cases can be traced back to a single culprit: atherosclerosis. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), approximately 90% of renal artery stenosis cases—a leading cause of renal hypertension—are directly linked to this condition.
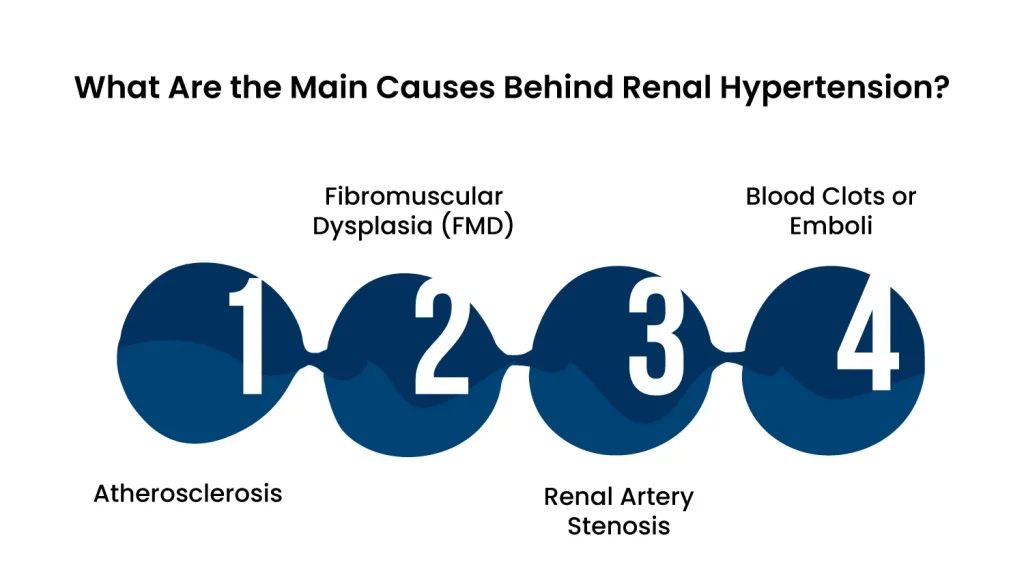
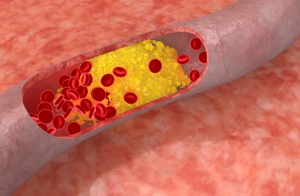
1. Atherosclerosis
Atherosclerosis is the most common cause of renal hypertension, especially in older adults. It occurs when fatty deposits (plaque) accumulate along the walls of the renal arteries, reducing blood flow. This condition often develops as a result of:
- High cholesterol levels
- Smoking
- Hypertension itself
- Advanced age
The reduced blood flow prompts the kidneys to activate the renin-angiotensin-aldosterone system (RAAS), raising blood pressure further.
2. Fibromuscular Dysplasia (FMD)
Fibromuscular dysplasia is a less common but significant cause, particularly in younger individuals and women. It involves abnormal growth or thickening of the artery walls, leading to narrowing or kinking of the renal arteries.
- Unlike atherosclerosis, FMD is not caused by plaque buildup.
- The exact cause is unknown, but it may be linked to genetic or hormonal factors.
This condition disrupts kidney function and elevates blood pressure.
3. Renal Artery Stenosis
Renal artery stenosis is a broad term that encompasses both atherosclerosis and fibromuscular dysplasia. It refers to any condition that leads to narrowing of the renal arteries, ultimately restricting blood flow. The resulting ischemia (lack of oxygen) in the kidneys triggers high blood pressure as the body attempts to compensate.
4. Blood Clots or Emboli
In some cases, renal hypertension can arise from blood clots or emboli that block the renal arteries. These blockages are often sudden and can lead to a rapid increase in blood pressure. Potential causes include:
- Atrial fibrillation or other heart conditions
- Trauma or injury
- Clotting disorders
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsSymptoms of Renal Hypertension
The symptoms can be subtle and nonspecific, making it challenging to identify early. However, recognizing these signs is crucial for timely diagnosis and treatment.
Blood Pressure That Defies Control
One of the hallmark signs of renal hypertension is blood pressure that resists conventional treatment. Many individuals find their prescribed medications insufficient to bring their numbers down, with blood pressure consistently exceeding 140/90 mmHg. This relentless hypertension is often a clue that the kidneys may be involved.
Swelling in the Body
When the kidneys aren’t working well, extra fluid can build up in your body. This often causes swelling in the legs, feet, or abdomen. This swelling is called edema.
Feeling Tired or Weak
When your kidneys don’t work properly, they can’t remove waste from your body. This can make you feel unusually tired or weak, even if you’ve had enough rest.
Changes in Urine
Problems with kidney function can lead to noticeable changes in your urine. You might urinate less than usual, see foam in your urine, or even notice blood in it.
Headaches and Dizziness
High blood pressure caused by renal hypertension can trigger frequent headaches or make you feel dizzy, especially when you stand up quickly or move suddenly.
Vision Problems
Very high blood pressure can damage the small blood vessels in your eyes. This might make your vision blurry or cause sudden vision loss in extreme cases.
Shortness of Breath
If your body retains too much fluid, it can build up in your lungs, making it hard to breathe. This symptom usually happens in more advanced stages of the condition.
How Common Is Renal Hypertension?
Renal hypertension is a relatively uncommon but serious condition that contributes to a subset of high blood pressure cases. It is estimated that 5–10% of hypertension cases are caused by problems with the renal arteries.
How Renal Hypertension Is Diagnosed?
Diagnosing renal hypertension requires a combination of clinical evaluation, blood pressure monitoring, and specialized tests to determine if kidney or blood vessel issues are contributing to high blood pressure. Since this condition often overlaps with essential hypertension, careful assessment by a healthcare provider is essential.
1. Medical History and Physical Examination
Medical History: A doctor will ask about your blood pressure history, family history of hypertension, and any symptoms such as swelling, fatigue, or vision changes.
Physical Exam: During the exam, the doctor may listen for abnormal sounds, called bruits, in the abdomen. These sounds can indicate narrowed renal arteries.
2. Blood and Urine Tests
Kidney Function Tests: Blood tests measuring creatinine and blood urea nitrogen (BUN) can reveal how well the kidneys are filtering waste.
Urinalysis: Tests for protein, blood, or other abnormalities in the urine can indicate kidney damage.
3. Blood Pressure Measurements
Persistent or resistant hypertension (blood pressure that remains high despite treatment with three or more medications) is a key sign that renal hypertension might be present.
Sudden onset of high blood pressure, especially in people under 30 or over 50, can also raise suspicion.
4- Imaging Tests for Renal Arteries
To confirm the diagnosis and identify narrowing or blockage in the renal arteries, doctors use imaging techniques, including:
Ultrasound with Doppler Imaging: This non-invasive test evaluates blood flow in the renal arteries and can detect narrowing.
CT Angiography (CTA): A detailed imaging test using contrast dye to visualize blood vessels.
Magnetic Resonance Angiography (MRA): A safer alternative to CTA for patients with kidney problems or those who can’t tolerate contrast dye.
Renal Arteriography: An invasive procedure that provides the most precise view of the renal arteries. It is usually performed when intervention, such as stenting, is being considered.
5. Specialized Diagnostic Tests
Plasma Renin Activity: Measures renin levels in the blood, which are often elevated in renal hypertension.
Captopril Renal Scan: A nuclear medicine test that assesses how well the kidneys function before and after taking captopril (a medication that affects blood pressure regulation).
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsWhen to Consider Renal Hypertension Testing
Testing for renal hypertension is often recommended when:
- High blood pressure is difficult to control with standard treatments.
- Blood pressure increases suddenly or severely, especially in younger or older individuals.
- Lab tests show unexplained kidney function decline or abnormal urine findings.
- There is a suspicion of renal artery stenosis due to underlying conditions like atherosclerosis or fibromuscular dysplasia.
Treatment Options for Renal Hypertension
The goal of treating renal hypertension is to manage high blood pressure, restore proper blood flow to the kidneys, and prevent complications such as kidney failure or cardiovascular issues
1. Medications to Control Blood Pressure
Medications are often the first line of treatment for renal hypertension. These include:
- Angiotensin-Converting Enzyme (ACE) Inhibitors or Angiotensin II Receptor Blockers (ARBs): These drugs help lower blood pressure by relaxing blood vessels and reducing the kidney’s release of renin. Examples include lisinopril and losartan.
- Calcium Channel Blockers: Medications like amlodipine relax blood vessel walls to improve blood flow.
- Beta-Blockers: These reduce heart rate and lower blood pressure.
- Diuretics: Often referred to as “water pills,” these help remove excess fluid and reduce swelling.
2. Lifestyle Changes
Lifestyle modifications play a crucial role in managing renal hypertension and preventing its progression:
- Dietary Adjustments: A low-sodium, heart-healthy diet such as the DASH (Dietary Approaches to Stop Hypertension) diet can help reduce blood pressure.
- Regular Exercise: Engaging in moderate physical activity, like walking or swimming, can improve heart health.
- Weight Management: Maintaining a healthy weight reduces the strain on the cardiovascular system.
- Smoking Cessation: Smoking worsens atherosclerosis and must be avoided to improve vascular health.
- Limiting Alcohol: Reducing alcohol intake can help control blood pressure.
3. Procedures to Restore Blood Flow
If renal hypertension is caused by significant narrowing of the renal arteries, interventional procedures may be necessary:
- Angioplasty and Stenting:
During this minimally invasive procedure, a small balloon is inflated inside the narrowed artery to widen it. A stent (a small mesh tube) is often placed to keep the artery open.
This is commonly used in cases of renal artery stenosis caused by atherosclerosis or fibromuscular dysplasia.
- Surgical Bypass:
In rare cases, bypass surgery may be performed to create an alternate route for blood flow around a severely narrowed or blocked renal artery.
This is generally reserved for complex cases where angioplasty is not feasible.
4. Treating the Underlying Cause
- Atherosclerosis: Managing cholesterol levels with medications (e.g., statins) and lifestyle changes can slow the progression of plaque buildup.
- Fibromuscular Dysplasia: Angioplasty without stenting is often effective for treating this condition.
- Blood Clots: Anticoagulants (blood thinners) may be prescribed to dissolve clots and prevent future blockages.
5. Dialysis or Kidney Transplant
In cases where renal hypertension leads to advanced kidney failure, dialysis or a kidney transplant may become necessary. These options are considered when kidney damage is irreversible and other treatments are no longer effective.
Words By Author
Renal hypertension directly links your kidney health to high blood pressure, making early detection and treatment essential. By recognizing the symptoms and understanding the causes, you can take proactive steps to protect your kidney function and overall health. If you suspect you might have renal hypertension, don’t wait—reach out to to cardiologist at Atlantic Cardiovascular to learn more about your condition and treatment options. Taking action now can make all the difference.