The human heart is enclosed in a protective sac called a pericardium, this sac plays an integral part in the proper functioning of the heart but what happens if the fluid begins to accumulate within the sac this often leads to serious complications ranging from mild to life-threatening.
Two such conditions are pericardial effusion and cardiac tamponade. Although both involve fluid accumulating around the heart, they represent distinct stages on a spectrum of severity.
In this blog post, we will explore the underlying causes of pericardial effusion and cardiac tamponade, we will explore the difference between these two conditions. Let’s begin our exploration of these two critical conditions that can impact the heart’s ability to function optimally.
What is Pericardial Effusion?
Pericardial effusion, in essence, is the abnormal accumulation of fluid within the pericardial cavity – the space between the heart and the pericardium. The pericardium, a two-layered sac, plays a crucial role in protecting and supporting the heart. Normally, a small amount of fluid exists within this cavity to facilitate smooth heart movement.
What is Cardiac Tamponade?
Cardiac tamponade represents a critical and potentially life-threatening complication of pericardial effusion. It occurs when the fluid buildup within the pericardial sac becomes so significant that it exerts excessive pressure on the heart. This pressure restricts the heart’s ability to fill with blood adequately, leading to a cascade of circulatory problems.
In essence, cardiac tamponade is a state of circulatory shock caused by the compression of the heart. The heart, unable to expand fully, cannot pump enough blood to meet the body’s needs. This can lead to a rapid decline in blood pressure, organ dysfunction, and, if left untreated, cardiac arrest.
Causes of Pericardial Effusion
Pericardial effusion can arise from a variety of underlying factors that disrupt the normal balance of fluid within the pericardial cavity
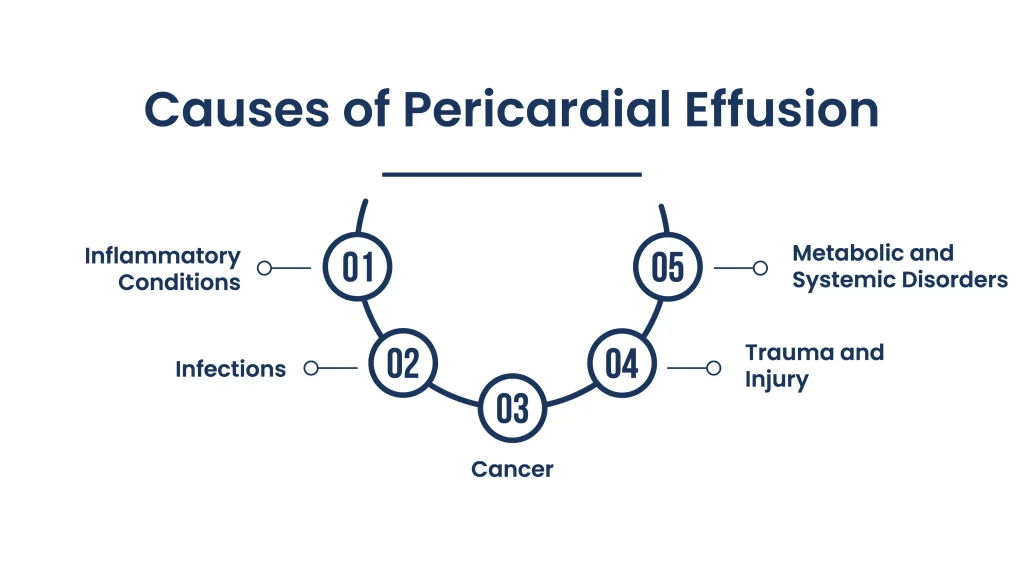
1. Inflammatory Conditions
- Pericarditis: Inflammation of the pericardium, often triggered by infections (viral, bacterial, fungal), autoimmune diseases (lupus, rheumatoid arthritis), or even certain medications, is a common culprit behind pericardial effusion.
- Post-cardiac Injury Syndrome: This inflammatory response can occur after heart surgery, heart attacks, or other procedures that injure the pericardium.
2. Infections
- Viral Infections: Viruses like HIV, coxsackievirus, and echovirus can directly infect the pericardium, leading to inflammation and fluid buildup.
- Bacterial Infections: Tuberculosis and other bacterial infections can also cause pericarditis and subsequent effusion.
3. Cancer
- Primary Cardiac Tumors: Although rare, tumors originating in the heart itself can cause pericardial effusion.
- Metastatic Cancer: Cancer that spreads from other organs, particularly lung, breast, and lymphoma, can invade the pericardium, leading to fluid accumulation.
4. Trauma and Injury
- Chest Trauma: Blunt or penetrating injuries to the chest, such as from accidents or surgery, can cause bleeding into the pericardial cavity.
- Aortic Dissection: A tear in the inner layer of the aorta can lead to blood leaking into the pericardial sac.
5. Metabolic and Systemic Disorders
- Kidney Failure: Impaired kidney function can lead to fluid retention throughout the body, including the pericardial cavity.
- Hypothyroidism: Underactive thyroid can also contribute to fluid buildup.
- Connective Tissue Disorders: Conditions like lupus and scleroderma can affect the pericardium and lead to effusion.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsHow Cardiac Tamponade Develops
Cardiac tamponade is a critical consequence of pericardial effusion, but it doesn’t always occur. Understanding how it develops is vital in recognizing its potential severity.
The Progression from Effusion to Tamponade
Pericardial effusion begins with the abnormal buildup of fluid within the pericardial sac. This can happen gradually or rapidly, depending on the underlying cause.
As the fluid volume increases, it starts to exert pressure on the heart. Initially, the pericardium may stretch to accommodate some extra fluid, but its capacity is limited.
Once the pressure exceeds a certain threshold, it starts to impede the heart’s ability to fill with blood during diastole (the relaxation phase). The heart chambers, particularly the right atrium and ventricle, become compressed.
With restricted filling, the heart’s pumping capacity diminishes, leading to a decrease in cardiac output – the amount of blood pumped out with each heartbeat.
Reduced cardiac output results in inadequate blood flow to the body’s organs and tissues. This triggers a cascade of compensatory mechanisms, such as increased heart rate and constriction of blood vessels, in an attempt to maintain blood pressure.
If the pressure continues to rise unabated, the heart becomes severely compressed, and cardiac output plummets further. This critical state is known as cardiac tamponade. It can lead to shock, organ failure, and, if left untreated, cardiac arrest.
Key Symptoms and Signs of Cardiac Tamponade
While some symptoms overlap with those of pericardial effusion, certain signs are more indicative of tamponade.
Beck’s Triad: This classic triad of symptoms is highly suggestive of tamponade, though not always present in every case:
- Hypotension (Low Blood Pressure): The heart’s compromised pumping ability leads to a significant drop in blood pressure.
- Distended Neck Veins (Jugular Venous Distension): Increased pressure in the chest causes the veins in the neck to become visibly swollen.
- Muffled Heart Sounds: The fluid surrounding the heart dampens the sounds of the heartbeat, making them difficult to hear with a stethoscope.
Pulsus Paradoxus: This is a drop in systolic blood pressure of more than 10 mmHg during inhalation. It occurs because the increased pressure in the chest during inspiration further restricts the heart’s filling.
Tachycardia (Rapid Heart Rate): The heart may try to compensate for reduced output by beating faster.
Rapid Breathing (Tachypnea): The body tries to compensate for decreased oxygen delivery by increasing the breathing rate. Patients may feel short of breath, even at rest.
What to Do If You Suspect Tamponade
Once the person arrives at the hospital, the medical team will act quickly to diagnose and treat tamponade.
- STAT Bedside Echocardiogram: An echocardiogram (ultrasound of the heart) will be performed immediately to confirm the presence of pericardial effusion and assess the heart’s function. Key findings suggestive of tamponade include:
- Pericardial effusion
- Increased respiratory variation in mitral and tricuspid inflow
- Diastolic collapse of the right atrium and right ventricle
- Dilated inferior vena cava
- Pericardiocentesis: If tamponade is confirmed, a procedure called pericardiocentesis may be performed. This involves inserting a needle into the pericardial sac to drain the excess fluid, relieving pressure on the heart. This procedure can be life-saving.
- Other Interventions: Depending on the underlying cause of the tamponade, additional treatments may be necessary. These might include surgery to repair a ruptured blood vessel, medications to treat inflammation or infection, or even chemotherapy or radiation therapy for cancer.
Treatment Options for Cardiac Tamponade
Cardiac tamponade is a medical emergency, and the primary goal of treatment is to relieve the pressure on the heart and restore adequate blood flow. Several approaches can be utilized, depending on the severity of the tamponade and the underlying cause.
1. Pericardiocentesis
- Procedure: This involves inserting a needle into the pericardial sac, typically guided by echocardiography, to drain the excess fluid.
- Benefits:
- Immediate relief of pressure on the heart
- Relatively quick and minimally invasive
- Can be performed at the bedside in emergency situations
- Considerations:
- May require a catheter to be left in place for continued drainage
- Carries a small risk of complications, such as bleeding or puncture of the heart or lung
2. Pericardial Window
- Procedure: A surgical procedure where a portion of the pericardium is removed, creating a “window” to allow fluid to drain freely into the chest cavity.
- Benefits:
- Prevents fluid from reaccumulating
- May be preferred for recurrent effusions or certain underlying causes
- Considerations:
- More invasive than pericardiocentesis
- Requires general anesthesia
3. Other Supportive Measures
While awaiting definitive treatment or in cases of less severe tamponade, supportive measures may be employed:
- Intravenous Fluids: To increase blood volume and help maintain blood pressure.
- Vasopressors: Medications to constrict blood vessels and raise blood pressure.
- Oxygen Therapy: To ensure adequate oxygen delivery to the body’s tissues.
- Pain Management: To alleviate any associated chest pain or discomfort.
Words By Author
Understanding the distinction between pericardial effusion and cardiac tamponade is paramount in recognizing when a relatively benign condition escalates into a life-threatening emergency. While both involve fluid accumulation around the heart, tamponade’s impact on cardiac function demands swift and decisive action.
By remaining vigilant for the signs and symptoms of tamponade and seeking immediate medical attention, we can empower ourselves to protect the heart’s delicate balance and safeguard our well-being. Remember, when it comes to matters of the heart, knowledge and timely intervention can make all the difference.