“How long can the heart stop before you die?” It’s a simple question with a multifaceted answer. The duration a person can survive without a heartbeat depends on numerous factors, from the underlying cause of the arrest to the speed of medical intervention. Join us as we explore the delicate balance between life and death and uncover just how long the heart can pause before the clock runs out.
The Physiology of Cardiac Arrest
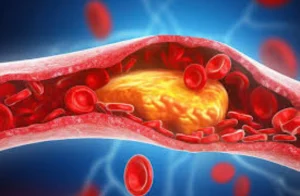
To understand how long the heart can stop before death occurs, we must grasp how it usually works. Your heart is a muscular pump divided into four chambers. It contracts rhythmically, sending oxygen-rich blood throughout your body and returning oxygen-depleted blood to the lungs for replenishment. This continuous cycle is essential for life.
When the Heart Stops
The “4-minute window” is a widely recognized concept in cardiac arrest care, referring to the crucial timeframe after the heart stops beating, in which intervention can significantly impact survival and neurological outcomes.
Cardiac arrest disrupts this finely tuned system. It’s not a heart attack (which involves a blockage in blood flow to the heart muscle). Instead, it’s an electrical malfunction where the heart’s rhythm becomes chaotic or ceases altogether. Without a coordinated beat, the heart can’t effectively pump blood.
4-Minute Window
This timeframe stems from the brain’s extreme sensitivity to oxygen deprivation. When the heart stops pumping blood, the brain is rapidly starved of oxygen, leading to cellular damage. After approximately 4-6 minutes, irreversible brain damage can begin to occur. The first few minutes after cardiac arrest are often called the “golden minutes.”
Stages of Cardiac Arrest
Cardiac arrest unfolds in stages, each marked by worsening physiological decline:
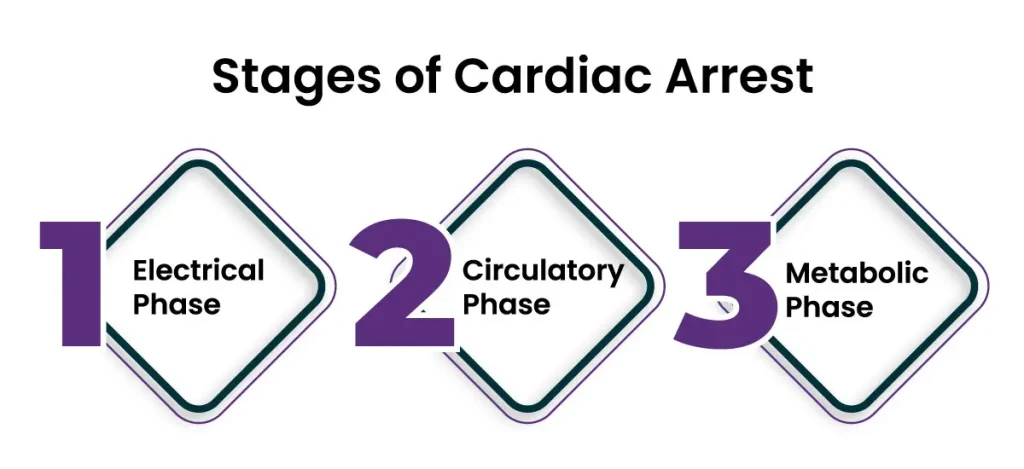
- Electrical Phase: The initial electrical malfunction (e.g., v-fib) disrupts the heart’s rhythm.
- Circulatory Phase: The ineffective heart contractions lead to a rapid drop in blood pressure and circulation.
- Metabolic Phase: Without oxygen, cells resort to anaerobic metabolism, producing harmful byproducts and further damaging tissues.
Cardiac Arrest Effect On Brain
The brain is the most sensitive organ to oxygen deprivation. Within seconds of cardiac arrest, brain function begins to deteriorate. After about 4-6 minutes, irreversible brain damage can start to occur. This is often referred to as the “4-minute window,” highlighting the critical need for rapid intervention.
Timeline of Brain Damage:
- 0-4 minutes: Brain cells begin to die, but damage may be reversible.
- 4-6 minutes: The risk of permanent brain damage increases significantly.
- 6-10 minutes: Widespread brain damage becomes highly likely.
- 10+ minutes: Survival with good neurological function becomes increasingly rare.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsWhat Happens If Your Heart Stops Beating for 10 Seconds?
If your heart stops beating for 10 seconds, you’ll likely experience lightheadedness or dizziness, and you may even briefly lose consciousness. This is because the sudden lack of blood flow to the brain deprives it of oxygen, which is essential for its function.
Here’s a more detailed breakdown of what happens:
- 0-5 seconds: You’ll likely feel dizzy or lightheaded as blood pressure drops and less oxygen reaches your brain.
- 5-10 seconds: You may lose consciousness as your brain temporarily shuts down due to lack of oxygen.
- After 10 seconds: If your heart doesn’t restart on its own, you’ll remain unconscious and may experience seizures. Without immediate intervention (CPR), permanent brain damage can begin within minutes.
While a 10-second pause in your heartbeat can be frightening, it’s usually not fatal if it restarts on its own or with prompt medical attention. However, every second counts when the heart stops. If someone collapses and loses consciousness, it’s crucial to:
- Call for emergency medical help immediately.
- Begin CPR (if trained) to manually pump blood and deliver oxygen to the brain.
- Use an AED (automated external defibrillator) if available to shock the heart back into a normal rhythm.
The sooner these interventions are initiated, the higher the chances of survival with minimal or no brain damage.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsHow CPR and AEDs Work to Reverse Cardiac Arrest?
CPR and AEDs are the two primary interventions for cardiac arrest, and they work in tandem to increase the chances of survival.
CPR, or cardiopulmonary resuscitation, is a manual technique that involves chest compressions and rescue breaths. Here’s how it works:
- Chest Compressions: By rhythmically pressing down on the chest, CPR mimics the heart’s pumping action. This helps circulate oxygenated blood to the brain and other vital organs, even if the heart isn’t beating effectively.
- Rescue Breaths: These breaths deliver oxygen to the lungs, which then enters the bloodstream and further helps to oxygenate the body.
While CPR doesn’t restart the heart, it buys crucial time by delaying brain damage and keeping the body alive until more definitive treatment can be provided.
AEDs, or automated external defibrillators, are portable devices that analyze your heart’s rhythm and deliver an electric shock (defibrillation) if necessary. This shock can interrupt the chaotic electrical activity in the heart during cardiac arrest and allow it to regain a normal rhythm.
Here’s how AEDs work:
- Analysis: The AED’s pads, placed on the victim’s chest, assess the heart’s rhythm.
- Decision: The AED determines if a shock is needed.
- Shock Delivery: If advised, the AED delivers a controlled electric shock to the heart.
CPR and AEDs work hand-in-hand to combat cardiac arrest. CPR maintains blood flow and oxygen delivery to the brain, while the AED attempts to restore a normal heart rhythm. The combination of these two interventions is the most effective way to increase the chances of survival and minimize brain damage.
Words By Author
The key takeaway is that time is of the essence in cardiac arrest. Every second counts. By understanding the physiological changes that occur when the heart stops and the lifesaving potential of CPR and AEDs, you can be empowered to act quickly and potentially save a life.
While the often-cited “4-minute window” serves as a stark reminder of the urgency of cardiac arrest, it’s not an absolute limit. Factors like age, underlying health, and even environmental temperature can influence how long the brain can withstand oxygen deprivation. Remember, learning CPR and familiarizing yourself with AEDs is an investment in the well-being of your community. You never know when you might be called upon to make a difference.