Aortic stenosis is a condition that often sneaks up quietly, gradually narrowing the valve that regulates blood flow from your heart. Whether you’ve recently been diagnosed or are supporting a loved one who is, it’s natural to wonder: How quickly will this condition get worse?
For some, the journey with aortic stenosis can span years with minimal changes. For others, the condition may progress more rapidly, leading to noticeable symptoms like shortness of breath, chest discomfort, or fatigue. Understanding how this progression unfolds is key to making informed decisions about monitoring, treatment, and lifestyle adjustments.
In this article, we’ll take a closer look at the progression of aortic stenosis, blending research-backed insights with practical information. Whether you’re someone just stepping into this journey or simply curious to understand the condition better, our goal is to offer clarity and guidance.
Does Aortic Stenosis Progress Quickly or Slowly?
One of the most common questions after a diagnosis of aortic stenosis is whether the condition will progress quickly or slowly. The truth is, there isn’t a one-size-fits-all answer. The rate of progression can vary widely between individuals, influenced by factors such as the severity of the condition at diagnosis, age, overall health, and even genetic predispositions.
In many cases, aortic stenosis progresses slowly over several years, especially if it is mild at the time of diagnosis. During this stage, you might not notice significant symptoms, and regular monitoring by your healthcare provider is often enough to keep things on track. However, as the condition advances from mild to moderate and eventually severe, the pace of progression can accelerate.
It’s important to understand that even in its early stages, aortic stenosis isn’t a condition to ignore. While some may experience gradual changes, others may find that symptoms—such as fatigue, chest pain, or difficulty breathing—emerge more quickly than expected.
What Does Research Suggest About Aortic Stenosis Progression?
Research provides valuable insights into the progression of aortic stenosis, offering a clearer picture of what to expect. According to the Cleveland Clinic, studies using catheterization and echocardiographic techniques show that, on average, the valve area in individuals with aortic stenosis declines by approximately 0.1 to 0.3 square centimeters per year. This narrowing of the valve restricts blood flow from the heart, gradually increasing strain on the heart muscle.
Additionally, the systolic pressure gradient across the aortic valve—a measure of how hard the heart must work to pump blood—can rise by 10 to 15 mm Hg per year in many cases. This increased pressure often correlates with worsening symptoms, such as fatigue, chest pain, and shortness of breath.
It’s also worth noting that age plays a significant role in the progression of aortic stenosis. Older adults are at higher risk for faster progression, often due to age-related calcification and other comorbidities that exacerbate valve narrowing. This highlights the importance of regular follow-ups, especially for elderly patients, to track the condition and intervene before complications arise.
Understanding these research-backed trends underscores the need for vigilance and proactive management to address the condition as it evolves.
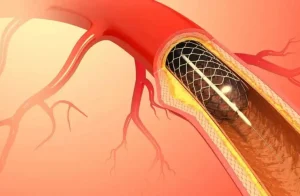
Stage-Wise Progression of Aortic Stenosis
Aortic stenosis progresses through well-defined stages, each with its own characteristics, symptoms, and management strategies. Understanding these stages can help patients and caregivers anticipate changes and work closely with healthcare providers to ensure timely interventions.
1. Mild Aortic Stenosis
- What Happens: In the early stage, the aortic valve begins to narrow, but blood flow is only slightly restricted. The heart can compensate for this change, so symptoms are often absent or minimal.
- Symptoms: Usually none; some patients may experience mild fatigue or shortness of breath during intense activity.
- Management: Regular monitoring through echocardiograms is essential to track the valve area and pressure gradients. Lifestyle changes and managing risk factors, such as high blood pressure, are often recommended.
2. Moderate Aortic Stenosis
- What Happens: The valve narrowing becomes more pronounced, making it harder for blood to flow. The heart begins to work harder to pump blood, which may lead to the thickening of the heart muscle (left ventricular hypertrophy).
- Symptoms: Some individuals may start noticing symptoms like mild shortness of breath or reduced exercise tolerance. However, others may remain asymptomatic.
- Management: More frequent monitoring is required. Depending on the patient’s health and symptoms, doctors may start preparing for potential future interventions, such as valve replacement.
3. Severe Aortic Stenosis
- What Happens: The aortic valve is significantly narrowed, leading to a major reduction in blood flow from the heart. This puts extreme strain on the heart, increasing the risk of complications such as heart failure.
- Symptoms: Noticeable symptoms include chest pain (angina), breathlessness, fatigue, dizziness, or fainting.
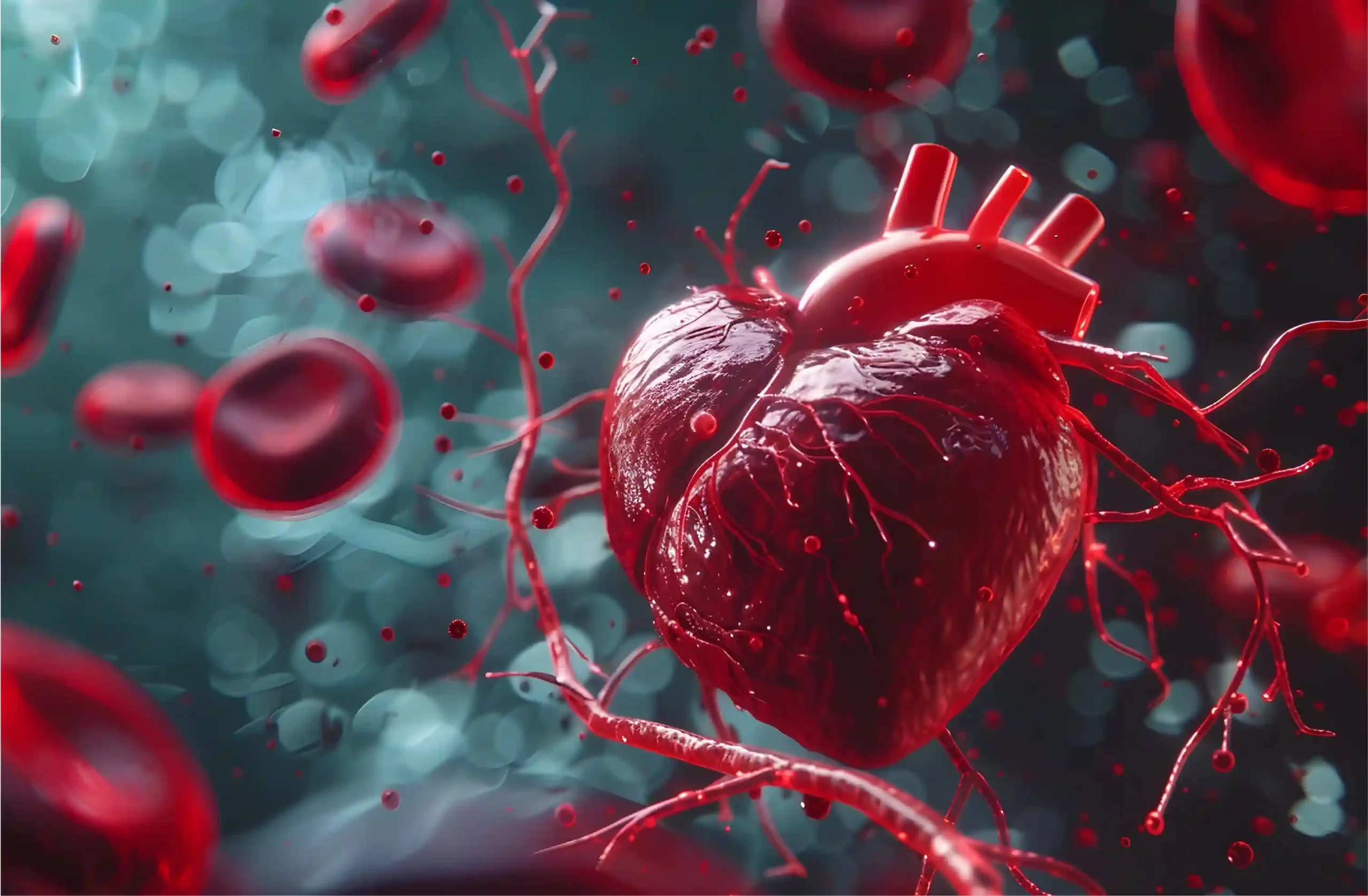
- Management: Severe cases often require surgical or minimally invasive interventions, such as aortic valve replacement (AVR) or transcatheter aortic valve replacement (TAVR). These treatments can significantly improve quality of life and outcomes.
4. Critical Aortic Stenosis
- What Happens: This is the final and most dangerous stage. The valve is critically narrowed, and the heart struggles to pump enough blood to meet the body’s needs.
- Symptoms: Symptoms are often severe and debilitating, including persistent breathlessness, chest pain, fainting, and swelling in the lower limbs. Risk of sudden cardiac death increases.
- Management: Immediate intervention is essential. Delaying treatment at this stage can result in life-threatening complications.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsLife Expectancy for People with Aortic Stenosis
Aortic stenosis is a serious condition, and its impact on life expectancy depends significantly on the stage of the disease and the presence of symptoms. Research underscores that individuals with severe symptomatic aortic stenosis are at the highest risk of sudden death. While sudden death is less common in asymptomatic cases, it is not entirely absent, highlighting the unpredictable nature of this condition.
Risk Across Stages
Progression rates vary widely, but those who experience rapid advancement to more severe stages of aortic stenosis typically face worse outcomes and higher mortality rates. According to the European Heart Journal, stages 4 and 5 of aortic stenosis are associated with the highest rates of death and complications, emphasizing the importance of timely intervention. Alarmingly, even in stage 1, research suggests a 9.2% mortality rate within the first year of diagnosis.
Treatment and Prevention
Currently, there are limited medical options to prevent, slow, or halt the progression of aortic stenosis. However, early diagnosis and timely intervention, particularly with valve replacement surgery such as surgical aortic valve replacement (SAVR) or transcatheter aortic valve replacement (TAVR), can significantly improve outcomes. These procedures are effective in preventing additional cardiac damage and improving life expectancy, especially in patients at high risk.
This underscores the importance of regular monitoring for anyone diagnosed with aortic stenosis, even in its earlier stages, to catch signs of progression early and ensure that interventions are carried out before complications arise.
Bottom Line
Aortic stenosis is a condition that demands vigilance, not fear. While the statistics and progression rates may seem daunting, advancements in modern medicine have dramatically improved outcomes for patients who seek timely care. The key lies in understanding the condition, staying proactive with regular check-ups, and exploring treatment options as they become necessary.