The words “heart failure” can strike fear into anyone’s heart. A diagnosis can feel like a life sentence, a countdown to an inevitable decline. But is that the whole story? Is there any hope for reversal, a chance to reclaim your health and vitality?
Let’s be honest, the answer isn’t a simple yes or no. Heart failure is a complex condition with varying causes and degrees of severity. But what we can say with certainty is this: there is more to the story than you may think.
In this guide, we’ll delve deep into the world of heart failure reversal. We’ll explore the latest research, lifestyle changes that can make a difference, and medical interventions that offer hope.
Can You Fully Recover From Heart Failure? (What Science Says)
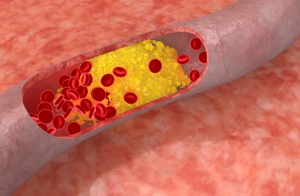
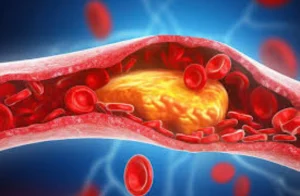
he million-dollar question on every heart failure patient’s mind. First, let’s clarify what we mean by “heart failure.” It doesn’t mean your heart has completely stopped working. Instead, it means your heart isn’t pumping blood as efficiently as it should. This can happen due to various reasons, like damage from a heart attack, high blood pressure, or underlying heart conditions.
Science reveals that a complete cure for heart failure isn’t always possible. However, constant adaptation to treatment can optimize cardiac functioning.
One thing is clear: early detection and intervention are key. If you experience symptoms like shortness of breath, fatigue, or swelling in your legs, don’t ignore them. Seek medical attention promptly. The sooner heart failure is diagnosed and treated, the better your chances of managing the condition and potentially reversing some of the damage.
What is Life Expectancy After Getting Diagnosed with Heart Failure?
it’s natural to wonder about the impact it will have on your lifespan. However, it’s important to remember that life expectancy after a heart failure diagnosis varies widely depending on several key factors.
Factors Influencing Life Expectancy:
- Severity of heart failure: The stage of heart failure at diagnosis plays a significant role. Early-stage heart failure generally has a better prognosis than advanced stage.
- Underlying cause: The underlying cause of heart failure can impact life expectancy. Some causes, like a reversible viral infection, may have a better outlook than others.
- Age and overall health: Younger patients and those with fewer underlying health conditions often have a better prognosis.
- Response to treatment: How well you respond to treatment, including medications, lifestyle changes, and potentially surgical interventions, can greatly influence your life expectancy.
Life Expectancy Statistics:
While individual experiences vary, research provides some general estimates:
- On average, about half of the individuals diagnosed with heart failure live for at least five years after diagnosis.
- Approximately 30% of individuals with heart failure live for 10 years or more.
- Life expectancy tends to be lower for older individuals and those with more advanced stages of heart failure.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsCan Heart Failure Be Reversed with Exercise?
The role of exercise in managing and potentially reversing heart failure is a topic of growing interest and research. While exercise alone may not completely reverse heart failure, especially in advanced stages, it can play a crucial role in improving heart function, quality of life, and overall prognosis.
Numerous studies have demonstrated the positive impact of exercise on heart failure outcomes:
A study published in the American Heart Association journal Circulation found that a year of exercise training helped improve heart muscle elasticity in people with early signs of heart failure.
Research suggests that exercise can reduce hospitalizations and mortality rates in heart failure patients.
A review of multiple studies concluded that exercise training improves exercise capacity, quality of life, and heart function in individuals with heart failure.
Can Heart Failure Be Reversed with Medication?
While medications cannot completely reverse the structural changes that have occurred in the heart due to heart failure, they can significantly improve heart function, manage symptoms, slow down the progression of the disease, and in some cases, lead to a partial reversal of heart failure.
Different types of medications work in various ways to address the underlying causes and effects of heart failure:
ACE inhibitors (Angiotensin-converting enzyme inhibitors) and ARBs (Angiotensin II receptor blockers): These medications help relax blood vessels, lower blood pressure, and reduce strain on the heart. Examples include lisinopril, enalapril, losartan, and valsartan.
Beta-blockers: These drugs slow down the heart rate, reduce blood pressure, and improve the heart’s pumping ability. Common beta-blockers used for heart failure include carvedilol, metoprolol, and bisoprolol.
Diuretics: These medications help eliminate excess fluid from the body, reducing swelling and easing the workload on the heart. Examples include furosemide, bumetanide, and spironolactone.
SGLT2 inhibitors (Sodium-glucose cotransporter-2 inhibitors): This newer class of drugs has shown promise in improving heart failure outcomes by lowering blood sugar levels and protecting the heart and kidneys. Examples include dapagliflozin and empagliflozin.
Natural Ways to Support Heart Health and Manage Heart Failure
While conventional medical treatments like medications and lifestyle changes are crucial for managing heart failure, there are several natural approaches that can complement these efforts and potentially contribute to improved heart health and quality of life. These natural strategies focus on holistic well-being and can be powerful tools in your heart failure management plan.
1. Prioritize Sleep:
Quality sleep is essential for overall health, and it plays a particularly important role in heart health. Aim for 7-8 hours of restful sleep each night. Establish a consistent sleep schedule, create a relaxing bedtime routine, and ensure your sleep environment is comfortable and conducive to rest.
2. Manage Stress:
Chronic stress can negatively impact heart health and exacerbate heart failure symptoms. Incorporate stress-management techniques into your daily routine. This could include meditation, yoga, deep breathing exercises, spending time in nature, listening to calming music, or engaging in hobbies you enjoy.
3. Embrace Relaxation Techniques:
Relaxation techniques like guided imagery, progressive muscle relaxation, and mindfulness can help reduce stress, lower blood pressure, and improve overall well-being. Consider exploring these practices with the guidance of a qualified practitioner.
Prevent heart problems before they start – Schedule a preventive checkup
Contact Us4. Quit Smoking:
Smoking is a major risk factor for heart disease and can worsen heart failure. If you smoke, quitting is one of the most important steps you can take to improve your heart health and overall well-being. Seek support from your doctor, a smoking cessation program, or resources like the National Quitline.
5. Prioritize Mental Health:
Living with heart failure can take an emotional toll. It’s important to address your mental health needs. Consider talking to a therapist or counselor who specializes in chronic illness. Therapy can provide valuable support, help you develop coping mechanisms, and improve your overall quality of life.