If you’ve ever sat in a cardiologist’s office, you’ve probably heard terms like atrial fibrillation and ventricular fibrillation thrown around. At first, they might just sound like medical jargon—but these heart rhythm issues are more than just fancy terms.
In fact, understanding the difference between them could be critical, especially if your heart health is already a concern. So, what exactly are AFib and VFib? And more importantly, which one should you be most worried about?
Let’s break it down together, so you’ll know what’s really going on with your heart and which type of fibrillation poses a bigger risk to your well-being.
What is Atrial Fibrillation?
Atrial fibrillation, or AFib, is a heart rhythm disorder that occurs when the upper chambers of your heart (the atria) beat irregularly and out of sync with the lower chambers (the ventricles). Normally, the heart beats in a steady rhythm, but with AFib, the atria start to quiver or “fibrillate,” creating a chaotic rhythm.
This erratic heartbeat means the atria can’t efficiently move blood into the ventricles, which can lead to blood pooling in the atria. The problem? Stagnant blood is more likely to form clots, which can travel to the brain and cause a stroke. AFib isn’t usually immediately life-threatening, but it can increase the risk of serious health issues like stroke, heart failure, and other complications if not managed properly.
What is Ventricular Fibrillation?
Ventricular fibrillation, or VFib, is a severe and often life-threatening heart rhythm disorder. Unlike atrial fibrillation, VFib occurs in the lower chambers of the heart, called the ventricles. These ventricles are responsible for pumping blood to the rest of your body. In VFib, these chambers start to quiver or “fibrillate” in an uncoordinated way, which means your heart isn’t able to pump blood effectively—or sometimes at all.
Without a steady heartbeat, your organs and tissues can’t get the oxygen-rich blood they need, and within minutes, this lack of blood flow can lead to sudden cardiac arrest and, if not treated immediately, death. That’s why VFib is considered a medical emergency requiring immediate action, such as CPR and defibrillation (using an electric shock to restart the heart).
Symptoms of Atrial Fibrillation (AFib)
AFib symptoms can vary from person to person. Some may experience noticeable symptoms, while others may not feel any symptoms at all, making AFib tricky to detect without a medical exam. Here are the most common symptoms associated with AFib:
- Irregular or Rapid Heartbeat: You may feel like your heart is racing, pounding, or fluttering.
- Shortness of Breath: You might feel breathless, especially during physical activity or even at rest.
- Fatigue: Many people with AFib feel unusually tired or have low energy levels.
- Dizziness or Lightheadedness: AFib can cause you to feel unsteady or like you might faint.
- Chest Discomfort: You may experience mild chest pain or a sensation of tightness.
While AFib is generally not immediately life-threatening, it can increase your risk of serious complications, such as stroke or heart failure, if left untreated.
Symptoms of Ventricular Fibrillation (VFib)
VFib, on the other hand, is much more dangerous and typically has sudden, severe symptoms. Because VFib interferes with the heart’s ability to pump blood, the symptoms are more intense and demand urgent action:
- Sudden Collapse: VFib often causes a person to suddenly lose consciousness due to a lack of blood flow to the brain.
- No Pulse or Heartbeat: VFib disrupts the heart’s pumping action entirely, leading to an absent or faint pulse.
- Loss of Consciousness: Because the heart stops pumping blood, fainting or sudden unconsciousness is common.
- Sudden Cardiac Arrest: VFib can quickly lead to cardiac arrest, meaning the heart stops beating altogether. Without immediate treatment, this can be fatal.
Since VFib symptoms usually occur abruptly and with little to no warning, it requires immediate emergency care, such as CPR or defibrillation, to restore a normal heart rhythm and potentially save a life.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsWhich is More Serious?
While both Atrial Fibrillation (AFib) and Ventricular Fibrillation (VFib) affect the heart’s rhythm and can lead to serious complications, VFib is generally considered far more dangerous due to its immediate life-threatening nature.
In VFib, the lower chambers of the heart (the ventricles) quiver instead of contracting effectively, which means the heart can’t pump blood to the rest of the body. Without blood flow, vital organs—especially the brain—are deprived of oxygen. As a result, VFib often leads to sudden cardiac arrest and, if not treated within minutes, can be fatal.
How Do the ECG Patterns Differ For Both?
- Irregularly Irregular Rhythm: The heart rate is irregular, meaning that there’s no consistent pattern to the timing of heartbeats.
- No P Waves: In a normal ECG, P waves represent the atrial contractions. In AFib, these are absent, as the atria are not contracting in a coordinated way.
- Fibrillatory Waves: Instead of P waves, you’ll see small, erratic, and rapid waves between each QRS complex (the main part of the heartbeat shown on an ECG). These waves represent the chaotic electrical activity in the atria.
- Variable QRS Complexes: The QRS complexes, which represent the ventricles contracting, occur at irregular intervals due to the erratic signaling from the atria.
Ventricular Fibrillation (VFib) ECG Pattern
- Chaotic, Disorganized Waves: VFib causes rapid, irregular, and chaotic waves across the entire ECG. There is no recognizable pattern or rhythm, as the ventricles are essentially “shaking” rather than contracting.
- Absence of QRS Complexes: Unlike AFib, VFib does not show distinct QRS complexes because the ventricles are not producing effective contractions. The electrical activity is so chaotic that no normal waveform can be identified.
- No P Waves or T Waves: Similar to the absence of QRS complexes, there are also no discernible P waves or T waves on the ECG, as the heart’s electrical system is in complete disarray.
How Cardiologist Daignoses AFib and VFib?
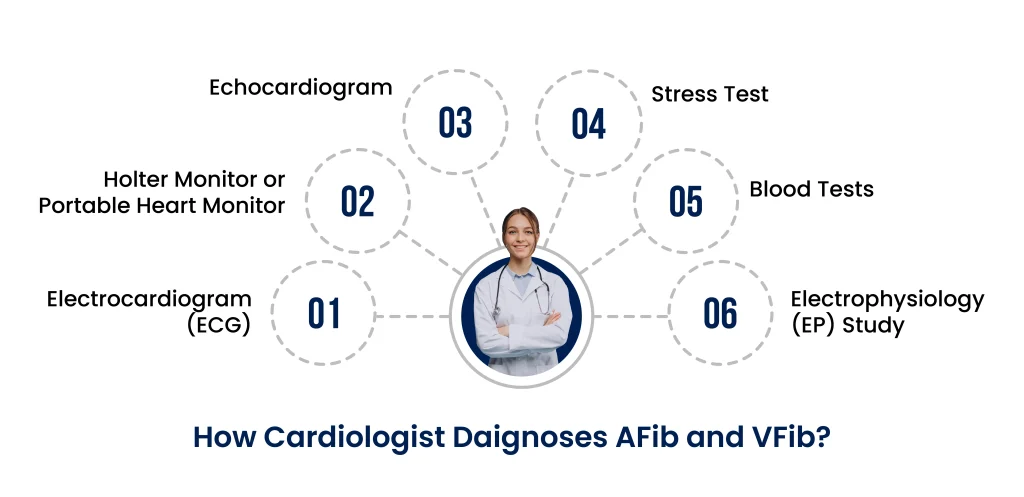
1. Electrocardiogram (ECG)
The ECG is the primary tool for diagnosing both AFib and VFib. It’s a quick, non-invasive test that records the electrical activity of the heart:
- For AFib: The ECG will show an irregular heartbeat with no distinct P waves, irregular R-R intervals, and fibrillatory waves. These characteristics allow cardiologists to confirm an AFib diagnosis, even if the patient isn’t experiencing symptoms at the time.
- For VFib: The ECG will display chaotic, disorganized waves without any recognizable QRS complexes, P waves, or T waves. VFib is generally diagnosed in emergency situations, as patients are often unresponsive due to cardiac arrest when this pattern is detected.
2. Holter Monitor or Portable Heart Monitor
For cases where AFib symptoms come and go, a standard ECG might not catch the abnormal rhythm. Cardiologists may recommend a Holter monitor or another type of portable heart monitor:
- Holter Monitor: This device continuously records heart activity over 24 to 48 hours, capturing irregular rhythms even if they only occur occasionally.
- Event Monitor: Similar to a Holter monitor but typically worn for a longer period (up to 30 days). The patient activates the monitor when symptoms occur, allowing cardiologists to pinpoint the heart’s activity during symptomatic episodes.
Since VFib is usually an immediate and life-threatening event, portable monitors are not typically used for VFib diagnosis; VFib requires emergency ECG confirmation.
3. Echocardiogram
An echocardiogram uses ultrasound to create an image of the heart. While this test doesn’t directly diagnose AFib or VFib, it provides important information about the heart’s structure and function:
- AFib: Cardiologists may use an echocardiogram to check for underlying issues, like valve problems or structural abnormalities, that could contribute to AFib. It can also help detect blood clots in the atria, which is critical for determining stroke risk.
- VFib: After a VFib episode, an echocardiogram might be used to assess any structural damage to the heart and identify underlying causes, such as a weakened heart muscle or previous heart attack damage.
4. Stress Test
A stress test involves monitoring the heart’s activity during exercise. While it’s not typically used to diagnose AFib or VFib directly, it can help uncover triggers or underlying conditions:
- AFib: A stress test might reveal AFib that’s brought on by physical exertion or stress, helping cardiologists understand if there are triggers that need to be managed.
- VFib: In patients with a history of VFib, a stress test is usually avoided due to the risk of triggering another episode. However, after stabilization, some patients undergo stress tests under controlled conditions to evaluate other heart-related risks.
5. Blood Tests
Blood tests are not used to diagnose AFib or VFib directly but can provide useful information to identify potential causes:
- AFib: Blood tests can detect thyroid dysfunction, electrolyte imbalances, and other issues that may contribute to AFib. They also help cardiologists determine if the patient is at risk for complications like stroke.
- VFib: For VFib, blood tests are often used in emergency settings to check for electrolyte abnormalities (like potassium imbalances) or cardiac markers indicating a heart attack.
6. Electrophysiology (EP) Study
An EP study is a more advanced diagnostic procedure where thin wires are threaded through a blood vessel to the heart to map its electrical signals.
- AFib: An EP study can identify the specific areas in the atria where abnormal signals are originating, which can help guide treatment, such as catheter ablation.
- VFib: This study is less commonly used for VFib due to the high risk involved. However, it may be done after stabilization to understand the underlying electrical disturbances in the ventricles and prevent future episodes.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsTreatments for Atrial Fibrillation (AFib)
AFib treatment aims to restore a normal heart rhythm, control the heart rate, and prevent complications like blood clots and stroke. Cardiologists may use a combination of medications, lifestyle changes, and procedures to manage AFib effectively.
1. Medications
Rate Control Medications
Rhythm Control Medications
Anticoagulants (Blood Thinners)
2. Cardioversion
In this procedure, a controlled electric shock is delivered to the heart to reset its rhythm. It’s done under sedation and often used when medications alone are not enough.
Antiarrhythmic drugs are administered to restore the heart’s normal rhythm. This can sometimes be done in a hospital setting under monitoring.
3. Catheter Ablation
In catheter ablation, thin wires (catheters) are threaded through blood vessels to the heart, where they deliver energy (like radiofrequency or cryotherapy) to destroy the small areas of heart tissue responsible for the abnormal electrical signals. This can be a long-term solution for some people with AFib who don’t respond well to medications.
4. Surgical Options
For cases where other treatments aren’t effective, surgical procedures like the Maze procedure may be considered. This involves creating a pattern of scar tissue in the heart that redirects electrical signals and helps restore normal rhythm.
Treatments for Ventricular Fibrillation (VFib)
VFib requires immediate emergency treatment, as it can lead to sudden cardiac arrest. The primary goal is to restore blood flow to vital organs by restarting the heart’s normal rhythm.
1. Emergency Treatment
When VFib occurs, CPR is essential to keep blood flowing to the brain and other organs until defibrillation can be performed.
An electric shock delivered via an external defibrillator (AED) or manual defibrillator is the standard treatment for VFib. This shock helps reset the heart’s electrical activity, allowing it to resume a normal rhythm.
2. Medications
- Antiarrhythmic Drugs
- Epinephrine
3. Implantable Cardioverter Defibrillator (ICD)
For people who have survived a VFib episode or are at high risk of recurrence, an ICD may be recommended. An ICD is a small device implanted under the skin that continuously monitors the heart’s rhythm and delivers a shock if it detects VFib or another dangerous rhythm. This can prevent sudden cardiac arrest in the future.
4. Catheter Ablation
In some cases, especially if VFib is caused by a specific area of abnormal electrical activity, catheter ablation may be performed to target and eliminate the problematic tissue. This procedure is less common for VFib but can be helpful for certain patients.
Ending Words
Understanding the differences between atrial fibrillation and ventricular fibrillation is crucial for managing your heart health. While AFib can increase your risk of stroke and other complications over time, VFib is a life-threatening emergency that requires immediate attention. Both conditions need proper medical management to minimize risks and improve quality of life.
If you or a loved one is experiencing symptoms of AFib or VFib, don’t wait. Reach out to the expert team at Atlantic Cardiovascular—they specialize in advanced diagnostics and personalized treatment plans for all heart rhythm disorders. With their guidance, you’ll have the support you need to take charge of your heart health and find peace of mind. Schedule a consultation today and start your journey toward a healthier heart.