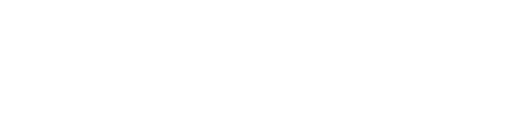
Cardiovascular disease remains one of the leading causes of death worldwide, and understanding the complexities of heart-related conditions is critical for effective prevention and treatment. Among the most commonly misunderstood terms are Coronary Artery Disease (CAD) and Acute Coronary Syndrome (ACS).
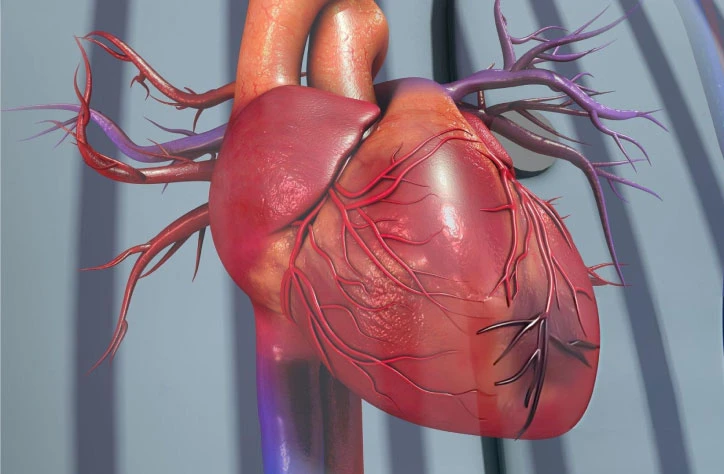
Coronary Artery Disease refers to the gradual buildup of fatty plaque in the coronary arteries, which can lead to narrowing and reduced blood flow over time. Acute Coronary Syndrome which is considered a type of CAD, is an umbrella term for a range of urgent conditions, including heart attacks (myocardial infarction) and unstable angina that occur when the plaque in the arteries ruptures or breaks, leading to a sudden blockage.
The confusion between CAD and ACS is not just semantic; it has real implications for diagnosis, treatment, and patient outcomes. Understanding CAD and its type are crucial for accurately assessing risk, customizing appropriate interventions, and ultimately improving cardiovascular health.
In this post, we will clarify these key distinctions, explain why the confusion persists, and provide a deeper understanding of how these conditions impact heart health.
Are CAD and ACS the Same Thing?
Although Coronary Artery Disease (CAD), Acute Coronary Syndrome (ACS), and are often used interchangeably in both medical discussions and general conversation, they are not the same. While these terms are all related to the broader category of cardiovascular disease, each represents a distinct clinical concept with different implications for diagnosis and treatment.
At its core, Coronary Artery Disease (CAD) refers to the progressive narrowing or blockage of the coronary arteries due to the buildup of fatty plaques (atherosclerosis). This gradual process reduces blood flow to the heart, increasing the risk of heart attacks, chest pain, and other cardiovascular complications. CAD is a long-term condition that can develop over many years, often without obvious symptoms until it reaches an advanced stage.
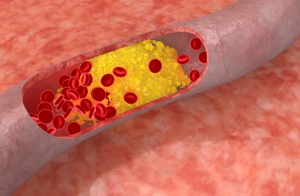
In contrast, Acute Coronary Syndrome (ACS) is a term used to describe a range of acute heart conditions that occur when a plaque in a coronary artery ruptures or breaks, leading to a sudden, complete blockage. This causes an abrupt reduction or cessation of blood flow to the heart muscle, often resulting in a heart attack or unstable angina (severe chest pain). In other words, ACS is a subset of CAD — it represents the acute, emergency phase of the disease when the underlying coronary artery blockages lead to immediate, life-threatening events.
The risk factors for Coronary Artery Disease (CAD) and Acute Coronary Syndrome (ACS) are largely overlapping, as both conditions are related to the buildup of plaque in the coronary arteries and the development of atherosclerosis. However, ACS occurs as a more acute event due to a sudden rupture or complication of existing plaque, whereas CAD refers to the ongoing process of artery narrowing over time. The following risk factors increase the likelihood of both CAD and ACS, but they may have different implications depending on the stage and progression of the disease.
Common Risk Factors for CAD and ACS
- High Blood Pressure (Hypertension)
- Effect on CAD: High blood pressure puts additional strain on the walls of the arteries, accelerating the process of atherosclerosis and increasing the likelihood of CAD over time.
- Effect on ACS: Hypertension increases the risk of plaque rupture and thrombosis (blood clot formation), which can trigger ACS events such as heart attacks and unstable angina.
- High Cholesterol Levels
- Effect on CAD: Elevated levels of LDL cholesterol (the “bad” cholesterol) contribute to the formation of fatty plaques in the arteries, a key driver of CAD.
- Effect on ACS: High cholesterol levels also promote plaque instability, making it more likely that plaque will rupture, leading to the acute events associated with ACS.
- Smoking
- Effect on CAD: Smoking damages blood vessels, increases cholesterol levels, and promotes inflammation, all of which contribute to the development of CAD.
- Effect on ACS: Smoking accelerates the rupture of atherosclerotic plaques and increases blood clotting, both of which are significant risk factors for ACS, especially heart attacks.
- Diabetes Mellitus
- Effect on CAD: Chronic high blood sugar levels damage the blood vessels and accelerate atherosclerosis, significantly increasing the risk of CAD.
- Effect on ACS: Diabetes is also associated with increased plaque formation and instability, making ACS events like heart attacks more likely.
- Obesity and Physical Inactivity
- Effect on CAD: Obesity is linked to other risk factors such as high cholesterol, hypertension, and diabetes, all of which contribute to the development of CAD.
- Effect on ACS: Obesity can increase the likelihood of plaque rupture and thrombosis, which can precipitate an ACS event, particularly when combined with other risk factors.
- Family History of Heart Disease
- Effect on CAD: A family history of early heart disease can increase your risk of developing CAD, as genetic factors play a significant role in cholesterol metabolism and vascular health.
- Effect on ACS: Having a family history of heart attacks or sudden cardiac events increases the risk of experiencing an ACS event, as genetic predisposition can lead to plaque instability.
- Age and Gender
- Effect on CAD: As we age, the risk of CAD increases, especially for men over the age of 45 and women after menopause, due to hormonal changes that affect lipid metabolism and vascular health.
- Effect on ACS: Age is also a critical factor in ACS risk. Older adults are at higher risk of experiencing an ACS event due to the natural progression of atherosclerosis and the increased fragility of blood vessels.
- Chronic Stress
- Effect on CAD: Chronic stress can contribute to high blood pressure, unhealthy eating habits, and other lifestyle factors that accelerate the development of CAD.
- Effect on ACS: Stress triggers the release of stress hormones like cortisol and adrenaline, which can increase blood pressure, inflammation, and the likelihood of plaque rupture, increasing the risk of ACS.
Types of CAD That Fall Under the Umbrella of ACS
1. Unstable Angina (UA)
- What it is: Unstable angina refers to chest pain that occurs unpredictably and is more severe than stable angina. Unlike stable angina, which is triggered by physical activity or stress, unstable angina can occur at rest or with minimal exertion. It is a warning sign of impending heart attack and is considered a medical emergency.
- How it fits under ACS: Unstable angina is part of the ACS spectrum because it is caused by a sudden reduction in blood flow to the heart, often due to the rupture of an atherosclerotic plaque and the formation of a partial blood clot. However, in unstable angina, the blockage does not cause permanent damage to the heart muscle (i.e., there is no myocardial necrosis).
- Symptoms: Chest pain that is more intense, lasts longer, and may occur at rest. It may be accompanied by shortness of breath, sweating, dizziness, or nausea.
- Treatment: Immediate treatment typically includes medications to manage symptoms and reduce the risk of progressing to a heart attack (e.g., blood thinners, nitroglycerin, beta-blockers). Patients with unstable angina often require hospitalization and monitoring.
2. Non-ST Elevation Myocardial Infarction (NSTEMI)
- What it is: NSTEMI is a type of heart attack that occurs when a coronary artery is partially blocked, leading to reduced blood flow and oxygen supply to the heart muscle. While NSTEMI causes damage to the heart muscle (myocardial injury), it does not cause the full-thickness damage associated with STEMI. NSTEMI is characterized by a lack of ST-segment elevation on an electrocardiogram (ECG), but the heart muscle is still damaged.
- How it fits under ACS: NSTEMI is classified under ACS because it involves an acute event triggered by the rupture of an atherosclerotic plaque and the formation of a blood clot that partially obstructs blood flow. Although the heart muscle is injured, it does not experience the same degree of damage as in STEMI.
- Symptoms: Chest pain, shortness of breath, sweating, nausea, and dizziness. Symptoms may be less intense or more intermittent than those seen with STEMI.
- Diagnosis and Treatment: NSTEMI is diagnosed through blood tests (elevated cardiac biomarkers like troponin) and ECG changes. Treatment usually involves a combination of antiplatelet agents, anticoagulants, and sometimes angioplasty or coronary artery bypass surgery (CABG) if necessary.
3. ST Elevation Myocardial Infarction (STEMI)
- What it is: STEMI is the most severe form of heart attack and occurs when a coronary artery is completely blocked, leading to a significant reduction or complete cessation of blood flow to a part of the heart muscle. This results in extensive heart muscle damage and is associated with ST-segment elevation on an ECG, which is a hallmark of STEMI.
- How it fits under ACS: STEMI is the most severe manifestation of ACS, representing an acute event where the rupture of a coronary plaque leads to total occlusion of the artery, resulting in irreversible damage to the heart muscle (myocardial infarction). Immediate intervention is required to restore blood flow and minimize long-term heart damage.
- Symptoms: Sudden, intense chest pain, often described as a crushing sensation, shortness of breath, sweating, nausea, dizziness, and sometimes loss of consciousness.
- Treatment: Treatment focuses on rapidly reopening the blocked artery. This may include thrombolytics (clot-busting drugs) or primary percutaneous coronary intervention (PCI) (angioplasty with or without stent placement). Timely intervention is critical to reducing heart muscle damage and improving outcomes.
Who Is at Risk of ACS?
While Acute Coronary Syndrome (ACS) is a sudden and potentially life-threatening condition, it is most often the result of the progression of CAD. The risk of developing ACS is highest in individuals with advanced or poorly managed CAD. However, ACS can affect anyone with underlying coronary artery disease, particularly if certain risk factors trigger an acute event.
1. People with Existing CAD
- Why? Individuals who have already developed CAD are at the highest risk of experiencing ACS. Plaque buildup over time can become unstable and rupture, leading to a heart attack (NSTEMI or STEMI) or unstable angina.
2. Men and Post-Menopausal Women
- Why? Men have a higher risk of ACS at an earlier age due to the lack of estrogen protection. However, post-menopausal women are at increased risk because estrogen levels drop, which can lead to changes in blood pressure, cholesterol, and other factors that affect heart health.
3. People with a History of Heart Attacks or Strokes
- Why? Those who have had a previous heart attack or stroke are at higher risk for further acute events, as their arteries may already be damaged, and they are more likely to experience plaque rupture.
4. People with Uncontrolled Risk Factors
- Why? Individuals with poorly managed high blood pressure, high cholesterol, diabetes, and smoking are at an increased risk of experiencing ACS. These risk factors contribute to the formation of unstable plaques that are prone to rupture and cause an acute coronary event.
5. People with Severe Atherosclerosis
- Why? The more severe the atherosclerosis (narrowing of the coronary arteries), the higher the likelihood that plaque will rupture and cause ACS. In advanced CAD, plaques become more unstable and prone to rupture.
6. Those with Multiple Risk Factors
- Why? The more risk factors you have, the greater the cumulative risk of developing ACS. For example, a combination of smoking, hypertension, high cholesterol, and obesity significantly increases the likelihood of an acute coronary event.
7. People with High Levels of Inflammation
- Why? Inflammation plays a key role in plaque instability. Conditions that promote systemic inflammation, such as autoimmune diseases (e.g., rheumatoid arthritis) or chronic infections, can increase the risk of ACS.
8. People with Stress-Induced Cardiac Events
- Why? Extreme stress or trauma can trigger ACS in susceptible individuals. Takotsubo cardiomyopathy (also known as “broken heart syndrome”) is an example of how severe emotional or physical stress can lead to an ACS event.
Treatment Options for ACS and CAD
The primary goals of treating Acute Coronary Syndrome (ACS) and Coronary Artery Disease (CAD) are to relieve symptoms and restore healthy blood flow to the heart muscle.
Medications for ACS and CAD
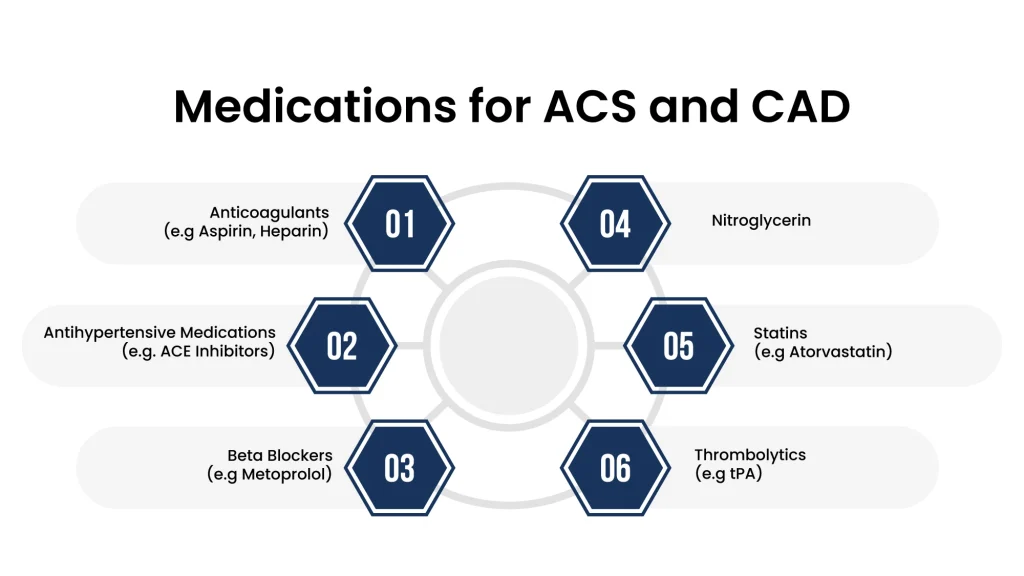
- Anticoagulants (e.g., Aspirin, Heparin)
- Purpose: Help dissolve existing clots or prevent new clots from forming, improving blood flow to the heart.
- Antihypertensive Medications (e.g., ACE Inhibitors)
- Purpose: Lower blood pressure, reducing strain on the heart and preventing further damage.
- Beta Blockers (e.g., Metoprolol)
- Purpose: Lower heart rate and blood pressure, easing the heart’s workload and reducing the risk of heart failure.
- Nitroglycerin
- Purpose: Dilates blood vessels to improve blood flow and relieve chest pain (angina).
- Statins (e.g., Atorvastatin)
- Purpose: Lower cholesterol levels, reducing the risk of plaque buildup and further blockage in the arteries.
- Thrombolytics (e.g., tPA)
- Purpose: Used in the hours following a heart attack to dissolve blood clots and restore blood flow, especially in STEMI cases.
Procedures for Treating ACS (Obstructive CAD)
- Angioplasty and Stent Placement
- What it is: A small mesh tube (stent) is inserted into a blocked coronary artery to widen it and improve blood flow. The procedure often involves inflating a balloon to compress the plaque and open the artery.
- Coronary Artery Bypass Grafting (CABG)
- What it is: A surgical procedure that uses a blood vessel from another part of the body (often the leg or chest) to bypass a blocked or narrowed coronary artery, restoring blood flow to the heart muscle.
Final Words
If you’ve been diagnosed with Coronary Artery Disease (CAD) or are at high risk for Acute Coronary Syndrome (ACS), it’s essential to take proactive steps to manage your heart health. With the right care and lifestyle changes, you can live a long, healthy life, even with a heart condition. Staying on top of your doctor appointments, following prescribed treatments, and adopting a heart-healthy lifestyle — including a nutritious diet, regular exercise, and stress management — are all key to reducing your risk of a heart attack and improving your overall well-being.At Atlantic Cardiovascular, we specialize in personalized care for individuals with CAD and ACS. Our expert team works with you to develop a tailored treatment plan that addresses your specific needs and helps you manage your condition effectively. Don’t wait to take action — your heart health matters, and we’re here to support you every step of the way.CContact us today to learn more about how we can help you live a healthier, heart-strong life.