Did you know millions of people have leaky heart valves and don’t even know it? Often, the symptoms creep in so subtly that they’re easy to overlook — a bit of fatigue, some shortness of breath, maybe a racing heartbeat after a simple walk. However when left untreated, a leaky heart valve can lead to serious heart complications.
In this post, we’ll unravel the mystery behind this common but often misunderstood heart condition. What causes a leaky heart valve? How can you spot the signs? And most importantly, what can you do to protect your heart from this silent threat? Get ready to learn everything you need to know about leaky heart valves.
What is a Leaky Heart Valve?
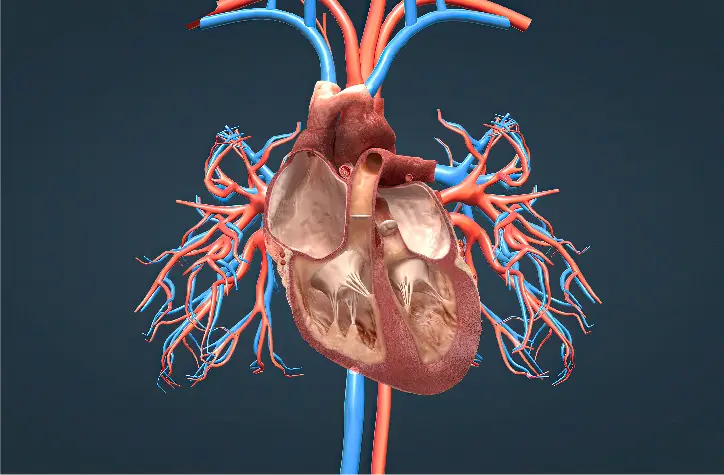
A leaky heart valve, also known as valve regurgitation, occurs when one of the heart’s valves doesn’t close properly, allowing blood to flow backward instead of moving forward as it should. This backward flow can reduce the heart’s efficiency, leading to symptoms that range from mild to severe, depending on the extent of the leakage and which valve is affected.
How Does It Work?
To understand a leaky heart valve, it helps to know a bit about how the heart works. The heart has four valves — the mitral, aortic, tricuspid, and pulmonary valves. These valves open and close with each heartbeat to keep blood moving in one direction through the heart’s chambers and out to the rest of the body.
When a valve is “leaky,” it means that the valve doesn’t close tightly enough. Instead of sealing completely, it allows some blood to slip back into the chamber it just left. This can force the heart to work harder to push enough blood through the body, potentially leading to symptoms and, over time, heart strain or enlargement.
Causes of a Leaky Heart Valve
Several factors can cause a leaky heart valve, including:
- Valve degeneration due to aging or wear and tear.
- Rheumatic fever or endocarditis (heart infections).
- Congenital heart defects (present at birth).
- Heart attack or other heart diseases that affect the heart’s structure.
- High blood pressure that puts strain on the heart over time.
Leaky heart valves can range in severity from mild (where you might not even notice any symptoms) to severe (which can lead to heart failure if not managed properly).
Why It Matters
While a mild leaky valve may not be a problem, a severe leak can disrupt normal blood flow and put a significant strain on the heart. Recognizing and addressing it early is key to maintaining heart health and preventing complications down the line.
How Is Leaky Heart Valve Diagnosed
Diagnosing a leaky heart valve often begins with a visit to your healthcare provider, who will evaluate your symptoms and listen to your heart. During a routine check-up, doctors can sometimes detect a leaky valve by hearing an abnormal sound, known as a heart murmur, through a stethoscope. However, to confirm the diagnosis and assess the severity, additional tests are typically needed. Here’s an overview of the most common methods:
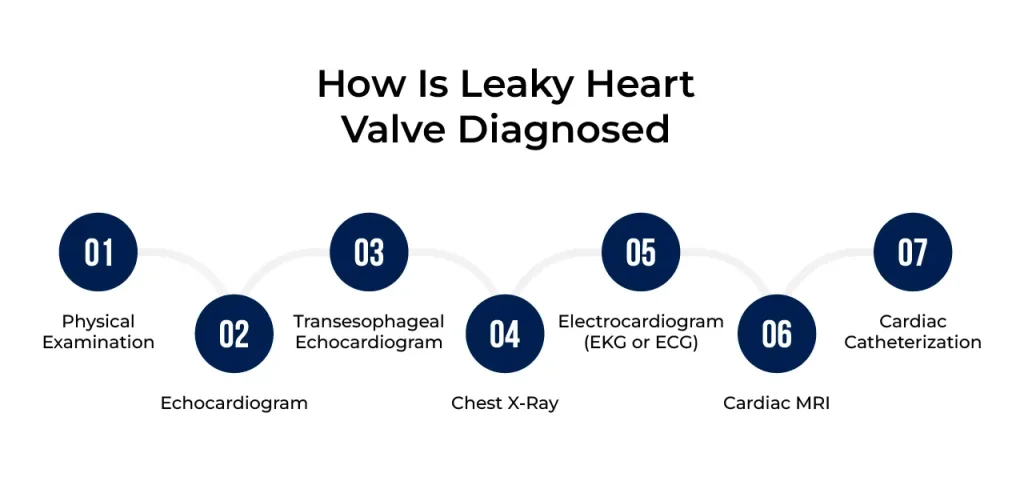
1. Physical Examination
- Listening for Murmurs: During a physical exam, your doctor will listen for heart murmurs, which are often the first clue that a valve may be leaking.
- Checking for Other Symptoms: The doctor may also check for signs of fluid retention, swelling, or irregular heart rhythms that could point to a leaky valve or other heart conditions.
2. Echocardiogram (Echo)
- This non-invasive ultrasound is one of the most important tools for diagnosing a leaky heart valve. It uses sound waves to create an image of your heart, allowing doctors to see the valves and chambers in action.
- With an echocardiogram, doctors can assess how well the valves are functioning, how much blood is leaking, and whether the heart has become enlarged due to the leakage.
- Doppler echocardiography is a specific type of echo that can measure the speed and direction of blood flow through the heart, which helps to pinpoint the severity of the leak.
3. Transesophageal Echocardiogram (TEE)
- A TEE is a specialized type of echocardiogram where the ultrasound probe is passed down the throat to get a closer look at the heart.
- This test provides clearer, more detailed images of the heart valves and is especially useful if the initial echocardiogram didn’t provide enough information or if doctors need to plan for surgery.
4. Chest X-Ray
- A chest X-ray can show the size and shape of your heart and check for fluid buildup in the lungs, which may indicate heart strain due to a leaky valve.
- While it doesn’t provide detailed information about the valves, it’s a helpful tool for assessing overall heart health and spotting related issues.
5. Electrocardiogram (EKG or ECG)
- An EKG measures the electrical activity of your heart and can detect irregular rhythms that might be caused by a leaky valve.
- It’s a quick, non-invasive test that helps doctors determine if the leakage is causing strain on the heart or leading to arrhythmias.
6. Cardiac MRI
- This imaging test provides highly detailed images of the heart and is sometimes used if an echocardiogram doesn’t give a complete picture.
- A cardiac MRI can show the structure and function of the heart in great detail, which can be useful for planning treatments or surgeries.
7. Cardiac Catheterization
- In some cases, particularly when the severity of the leakage is unclear or if surgical repair is being considered, a cardiac catheterization may be performed. This procedure involves inserting a thin tube (catheter) into a blood vessel and threading it to the heart.
- During the test, doctors can measure the pressure inside the heart chambers and visualize blood flow using a special dye and X-rays.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsThe Four Heart Valves and How They Can Leak (Regurgitation)
Each of the heart’s four valves has a crucial role in maintaining the one-way flow of blood through the heart’s chambers and out to the rest of the body. When any of these valves leak, it’s referred to as regurgitation, meaning blood is allowed to flow backward, disrupting the heart’s ability to pump efficiently. Here’s a closer look at each valve and how regurgitation can affect them:
1. Mitral Valve Regurgitation
The mitral valve is located between the left atrium and the left ventricle. It opens to allow blood to flow from the atrium to the ventricle and then closes tightly to prevent backflow. In mitral valve regurgitation, the valve fails to close completely, causing blood to leak backward into the left atrium each time the left ventricle contracts.
Causes:
Common causes include mitral valve prolapse (where the valve flaps bulge into the atrium), rheumatic heart disease, or damage from a heart attack. Mitral valve regurgitation is one of the most common types of valve issues.
Symptoms:
Fatigue, shortness of breath (especially when lying down), and heart palpitations are typical signs.
2. Aortic Valve Regurgitation
The aortic valve sits between the left ventricle and the aorta, which is the main artery that supplies oxygen-rich blood to the body. It opens to let blood flow from the heart to the aorta and then closes to prevent it from leaking back into the ventricle. Aortic valve regurgitation occurs when this valve doesn’t close properly, allowing blood to leak back into the left ventricle after each heartbeat.
Causes:
Aortic regurgitation can result from conditions such as aortic valve degeneration, congenital valve abnormalities (like a bicuspid aortic valve), high blood pressure, or infections that damage the valve tissue.
Symptoms:
This type of regurgitation can lead to chest pain, shortness of breath, and fatigue. Over time, it can cause the left ventricle to enlarge, potentially leading to heart failure if untreated.
3. Tricuspid Valve Regurgitation
The tricuspid valve is located between the right atrium and right ventricle, controlling blood flow between these chambers on the right side of the heart. Like the other valves, it should close tightly after blood passes through to prevent backflow. Tricuspid regurgitation happens when this valve leaks, allowing blood to flow backward into the right atrium when the right ventricle contracts.
Causes:
Often, tricuspid regurgitation is a result of right-sided heart failure, pulmonary hypertension (high blood pressure in the lungs), or damage from heart infections. It can also occur as a secondary effect from other valve disorders, like mitral valve regurgitation.
Symptoms:
This condition can cause symptoms such as swelling in the legs, abdominal discomfort, and a pulsing sensation in the neck veins.
4. Pulmonary Valve Regurgitation
The pulmonary valve sits between the right ventricle and the pulmonary artery, which carries blood to the lungs to pick up oxygen. It opens to allow blood to flow from the right ventricle into the pulmonary artery and then closes to prevent blood from flowing back. Pulmonary valve regurgitation occurs when the valve fails to close properly, allowing blood to leak back into the right ventricle.
Causes: This type of regurgitation is less common and often associated with pulmonary hypertension, congenital heart defects, or conditions like infective endocarditis. It may also develop as a result of previous heart surgery, especially if it involved the pulmonary artery or valve.
Symptoms: While mild cases may not cause symptoms, more severe cases can lead to shortness of breath, fatigue, and in some instances, chest pain or lightheadedness.
Prevent heart problems before they start – Schedule a preventive checkup
Contact UsTreatment Options for Leaky Heart Valve Disease
Treatment for a leaky heart valve, or valve regurgitation, depends on several factors, including the valve affected, the severity of the leakage, and the presence of symptoms. Mild cases may only require monitoring, while more severe cases might necessitate medications or surgery. Here’s a look at the primary treatment options available:
1. Monitoring and Lifestyle Changes
Regular Check-Ups: For mild or asymptomatic cases, regular monitoring is often the first step. Routine check-ups with a cardiologist and periodic imaging tests (like echocardiograms) help track any progression in valve regurgitation.
Lifestyle Modifications: Maintaining a heart-healthy lifestyle can help manage symptoms and prevent complications. This includes:
- Eating a balanced diet low in saturated fats and high in fruits, vegetables, and whole grains.
- Reducing salt intake to minimize fluid retention.
- Engaging in regular, moderate exercise to improve overall cardiovascular health (with guidance from a healthcare provider).
- Avoiding smoking and limiting alcohol intake.
Managing Other Health Conditions: Conditions like high blood pressure, diabetes, and high cholesterol can contribute to worsening valve issues. Managing these conditions with medication and lifestyle changes can help reduce strain on the heart.
2. Medications
Diuretics: These help reduce excess fluid in the body, which can alleviate symptoms such as swelling and shortness of breath. Diuretics are particularly helpful in cases where the valve regurgitation has led to heart failure symptoms.
Beta-Blockers: These medications help slow the heart rate and reduce blood pressure, lessening the workload on the heart. They can be beneficial in reducing symptoms and slowing the progression of valve disease.
ACE Inhibitors or ARBs: These drugs help relax blood vessels, reducing the pressure the heart has to work against. They are commonly prescribed if valve regurgitation has led to heart failure or other complications.
Blood Thinners (Anticoagulants): For some patients, particularly those with mitral valve regurgitation or those at risk for blood clots, blood thinners may be prescribed to prevent clots from forming.
3. Surgical Valve Repair
Valve repair is typically preferred over replacement whenever possible, as it preserves the patient’s own tissue and often has a quicker recovery time. Surgical repair techniques include:
- Annuloplasty: This involves placing a ring around the valve to tighten or reinforce it, helping it close more effectively and reducing regurgitation.
- Leaflet Repair: If the valve leaflets (flaps) are damaged or malformed, they can sometimes be reshaped, trimmed, or reinforced with tissue patches to improve their function.
- Chordal Repair: The chordae tendineae are tiny tendons that help the valve leaflets move. If they’re damaged, they can be shortened, repositioned, or replaced to improve valve closure.
4. Valve Replacement Surgery
In cases where the valve is too damaged to repair, valve replacement becomes necessary. The damaged valve is removed and replaced with either a mechanical valve or a biological (tissue) valve:
- Mechanical Valves: Made from durable materials like metal or ceramic, mechanical valves are designed to last a lifetime. However, they require patients to take blood-thinning medications for life to prevent blood clots.
- Biological Valves: These are made from animal or human tissue. While they do not typically require lifelong blood thinners, they may need to be replaced after 10 to 20 years as they gradually wear out.
Valve replacement is usually performed as open-heart surgery, although minimally invasive techniques are available in certain cases, leading to shorter recovery times.
5. Transcatheter Valve Procedures
For patients who may not be candidates for traditional surgery, transcatheter valve repair or replacement offers a less invasive option. This procedure involves threading a catheter (a thin, flexible tube) to the heart through a small incision, usually in the groin.
Common procedures include:
- Transcatheter Aortic Valve Replacement (TAVR): This technique is primarily used for aortic valve replacement and is a good option for high-risk patients.
- MitraClip: For mitral regurgitation, a small clip can be attached to the mitral valve via a catheter to help it close more effectively. This option is ideal for patients with severe mitral regurgitation who are too high-risk for surgery.
6. Future Treatments: Emerging Technologies
Medical advances are constantly expanding treatment options for valve regurgitation. Stem cell therapy, newly developed valve repair devices, and robot-assisted surgeries are just a few examples of emerging technologies that may offer innovative solutions in the future.
Ongoing clinical trials are exploring novel approaches to valve repair and replacement, giving patients more options and potentially improving outcomes.
Choosing the Right Treatment
The best treatment plan for valve regurgitation depends on individual factors, including the severity of the leakage, the specific valve affected, the patient’s overall health, and lifestyle preferences. Working closely with a cardiologist like those at Atlantic Cardiovascular can help patients make informed decisions about their care. Early intervention, regular monitoring, and tailored treatments can significantly improve quality of life and overall heart health for those with leaky heart valves.